Birth Control Can Be Effective With Lower Dosage Of Hormone
In an attempt to discover whether hormone levels may be decreased while still maintaining the effectiveness of contraceptives in delaying ovulation, researchers recently examined hormone levels in contraceptive devices.
Scientists from the University of the Philippines Diliman utilised computer modelling to calculate how much the hormone dosage may be decreased.

Their findings demonstrated that they could cut the hormone content of estrogen-only contraceptives by up to 92% while still preventing ovulation. Using hormonal contraceptives is a common way to avoid getting pregnant.
Though occasionally they can have negative consequences, this prompted a team of researchers in the Philippines to investigate whether it was possible to decrease the hormone dosage and timing of contraceptive pills while maintaining their effectiveness.
Their research, which was published in the journal PLOS Computational Biology, reveals that it is possible to significantly lower the hormone levels in both progesterone-only and estrogen-only contraceptives while still preventing ovulation.
Hormonal contraceptives working
Medical professionals frequently recommend hormonal contraceptives to female patients who want to avoid getting pregnant. In the United States, 10.3% of women use long-acting reversible contraceptives, while 12.6% of females between the ages of 15 and 49 use oral contraceptives, according to the Centres for Disease Control and Prevention (CDC).
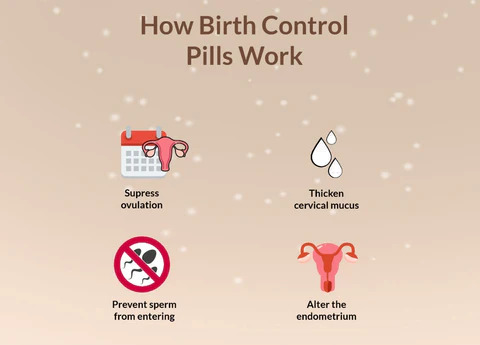
In order to prevent conception, hormonal contraceptive methods use artificial hormones like progesterone and oestrogen.
They may halt ovulation or thin the uterine lining to prevent an implanted egg from attaching, among other possible mechanisms of action.
Several hormonal contraceptive methods include pills, which can be progestin-only or a combination of hormones, arm implants (Nexplanon), contraceptive patches (Xulane), and intrauterine devices (IUDs) (Mirena or Skyla).
In addition to prescription contraceptives to prevent pregnancy, doctors occasionally do so to aid patients with polycystic ovarian syndrome (PCOS) in reducing the size of cysts and thereby lessening pain or in the treatment of endometriosis to aid in controlling pain and excessive bleeding.
The following negative effects of hormonal contraceptives can range from minor to severe:
- nausea
- headaches
- cramps in the stomach
- hypertension
- clots of blood
- stroke
The risk of deep vein thromboembolism, or leg blood clots, is also raised in people who smoke while using hormonal contraceptives.
Some milder side effects might fade disappear, but people should talk to their healthcare professionals about side effects to figure out the best course of action.
Reduction in hormone levels
The computer simulations demonstrated that ovulation can be prevented by adjusting the hormone amount.
Researchers discovered that it is possible to concentrate on changing the dose during specific times of the cycle and still have the contraceptives be effective, in addition to the fact that the models showed that hormones may be reduced.
The dosage for estrogen-only contraceptives was cut by 92% by the researchers while maintaining efficacy. They decreased the dose by 43% while maintaining the contraceptive effects of progesterone-only contraceptives.
When it comes to the time of hormone delivery, the authors state “that it is most effective to deliver the oestrogen contraceptive in the mid-follicular phase.”
Brenda Gavina, a PhD researcher at the University of the Philippines Diliman, discussed the study and went into more detail about its findings. She explained:
Theoretically, our mathematical model with the simplification assumptions revealed that as little as 10% of the total exogenous oestrogen dose in continual administration might provide contraception as long as this dosage is precisely scheduled, which was startling.
Benefits of lowering the dosage of hormones
Estradiol and progestin are often the main ingredients in oral contraceptives.
“Lowering the estradiol dose can increase breakthrough bleeding, efficacy in obese women, but decrease the risk of blood clotting,” stated Dr. Monte Swarup, FACOG, a board-certified OB/GYN and the creator of HPV HUB. “Estradiol increases proteins through its metabolism in the liver, including clotting proteins.”
Lowering the hormone dosage to the smallest effective level has various advantages.
According to Dr. Pamela Berens, professor of obstetrics, gynaecology, and reproductive sciences at McGovern Medical School at UTHealth Houston, “this reduces potential risks for both complications and side effects.
Blood clots (both deep venous clots in the legs, for example, and clots that affect the lung, such as pulmonary embolism), for example, are some major side effects of greater hormonal doses used in contraception.
Rare problems like heart attack, pulmonary embolism, and stroke are other dangers associated with blood clots. The risks of these uncommon but serious consequences are also decreased by reducing the hormone dosage.
Lower hormone levels also lessen the risk of more frequent side symptoms such nauseousness, breast tenderness, bloating, and irritability. According to Berens, the hormone doses in widely used birth control have decreased over time while maintaining their efficacy.
Timing the hormones matters
The study’s model also shown how crucial hormone timing is throughout the cycle.
It was particularly surprising, according to Gavina, that theoretically, our mathematical model (with the simplifying assumptions) demonstrated that as little as 10% of the total exogenous estrogen dose administered continuously could achieve contraception, provided that this dosage is administered at the exact right time (the timing was also demonstrated in our optimization result).
It’s crucial to keep in mind, though, that “the results of this study are not directly transferable to actual patients, but the principles proposed in our study could be easily translated,” as Gavina noted. We anticipate that these findings will help clinicians choose the best contraceptive dosage and regimen in order to use medications as effectively and efficiently as possible.
Additionally, timing the hormones aids in reducing bleeding. In perimenopause hormone replacement treatment, synchronising the hormones with the cycles reduces breakthrough or irregular bleeding, according to Swarup.
What do reproductive health experts think?
The study is not yet ready for clinical use, experts stressed, despite the fact that the findings suggest that altering the hormone dose in contraceptives is feasible while preserving efficacy.
The co-founder and CEO of Pandia Health in Sunnyvale, California, Dr Sophia Yen, a clinical associate professor at Stanford Medical School, who was not involved in the present study, said, “It’s important to realise that this [study finding] is theoretical and was not tested in humans.”
Dr. Yen added that “[the hormone level reduction] most likely won’t be so great for those with higher BMIs because of the greater volume of distribution for the drugs.”
The study’s results were also discussed by Dr. Sandra Hurtado, an assistant professor of obstetrics, gynaecology, and reproductive sciences at McGovern Medical School at UTHealth Houston who was not involved in its creation.
Dr. Hurtado made clear that the mathematical model used in the study needs to “undergo testing in an animal model and in humans to be able to test its safety and efficacy.”
She did recognise the study’s promise, though. Dr. Hurtado said, “It would be perfect if there was a mechanism to test and record the hormone levels in each individual and be able to give that person the dose at the right moment.
She added that carrying out this research further and creating tools like an automated insulin delivery system would be beneficial. “At this time, those are expensive and not justified for contraceptive use, but hopefully, it can be developed in the near future with continued advancements in technology and falling prices of electronics.”
REFERENCES:
- https://www.medicalnewstoday.com/articles/birth-control-with-up-to-92-lower-hormone-doses-could-still-be-effective
- https://www.healthline.com/health-news/birth-control-pills-might-be-able-to-work-with-92-fewer-hormones
- https://www.forbes.com/sites/anafaguy/2023/04/13/birth-control-can-be-effective-with-lower-dosage-of-hormones-study-finds/
- https://www.1news.co.nz/2023/04/17/the-pill-could-have-92-less-hormones-and-still-work-study-finds/
For Birth control medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=24