Expert note on causes of teeth sensitivity & its treatment.
When you have sensitive teeth, it can occasionally be uncomfortable to eat and drink. However, certain natural therapies might help lessen tooth sensitivity.
The condition of sensitive teeth is frequent and curable. One in eight patients who went to dental offices had sensitive teeth, according to a 2013 research.
What is Teeth Sensitivity?
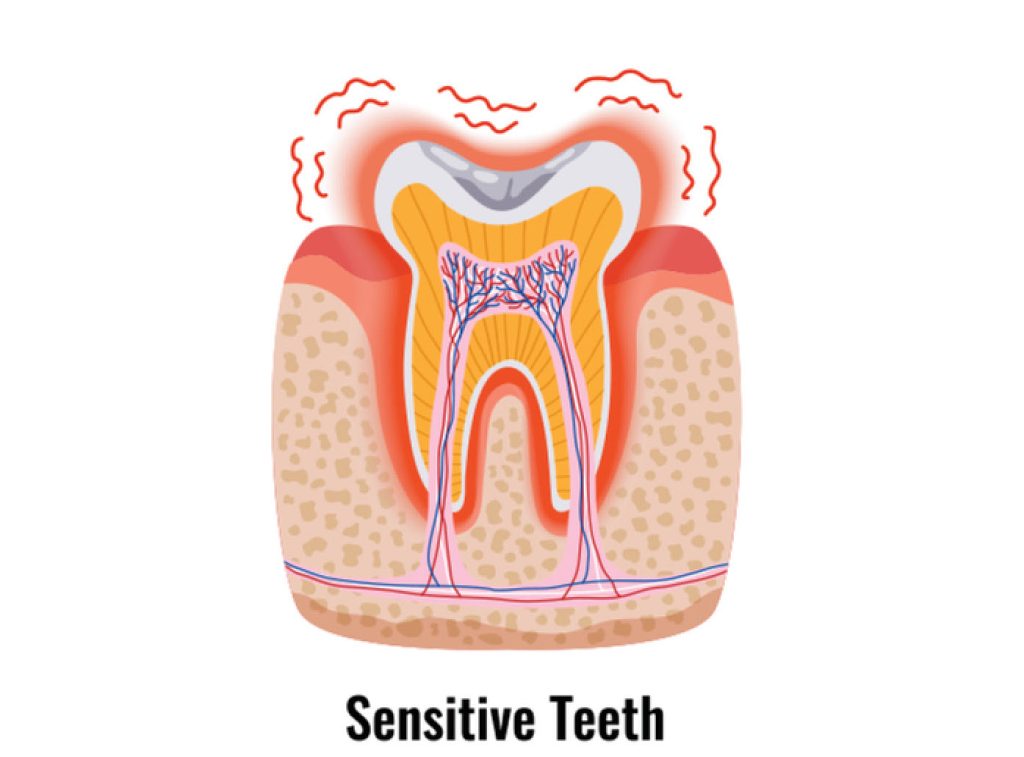
Dentin hypersensitivity, also known as tooth sensitivity, is what it means like. The teeth that become painful or uncomfortable in reaction to particular stimuli, such as hot or cold temperatures, causes sensitivity.
It can affect one tooth, many teeth, or all of the teeth in one person, and it can be a short-term or long-term issue. While sensitive teeth might have a variety of causes, the majority of them can be readily remedied by altering your oral hygiene routine.
Symptoms of sensitive teeth
People who have sensitive teeth may feel pain or discomfort when certain triggers are present. This discomfort may be felt at the tooth roots of the troubled teeth. Among the most typical triggers are:
- piping hot food and drink
- chilly foods and drinks
- chilly air
- sweet dishes and drinks
- sour foods and drinks
- especially while performing routine dental cleanings, cold water
- flossing or brushing your teeth
- Alcoholic mouthwashes
Over time, your symptoms could fluctuate without any apparent cause. They could be light or strong.
What causes tooth sensitivity?
The occurrence of sensitive teeth can be caused by a variety of circumstances, such as:
Brushing too strongly:
Over time, vigorous brushing or the use of a toothbrush with a firm bristle can wear down the enamel and expose the dentin. It might also result in gum recession (when your gum tissue pulls away from your teeth).
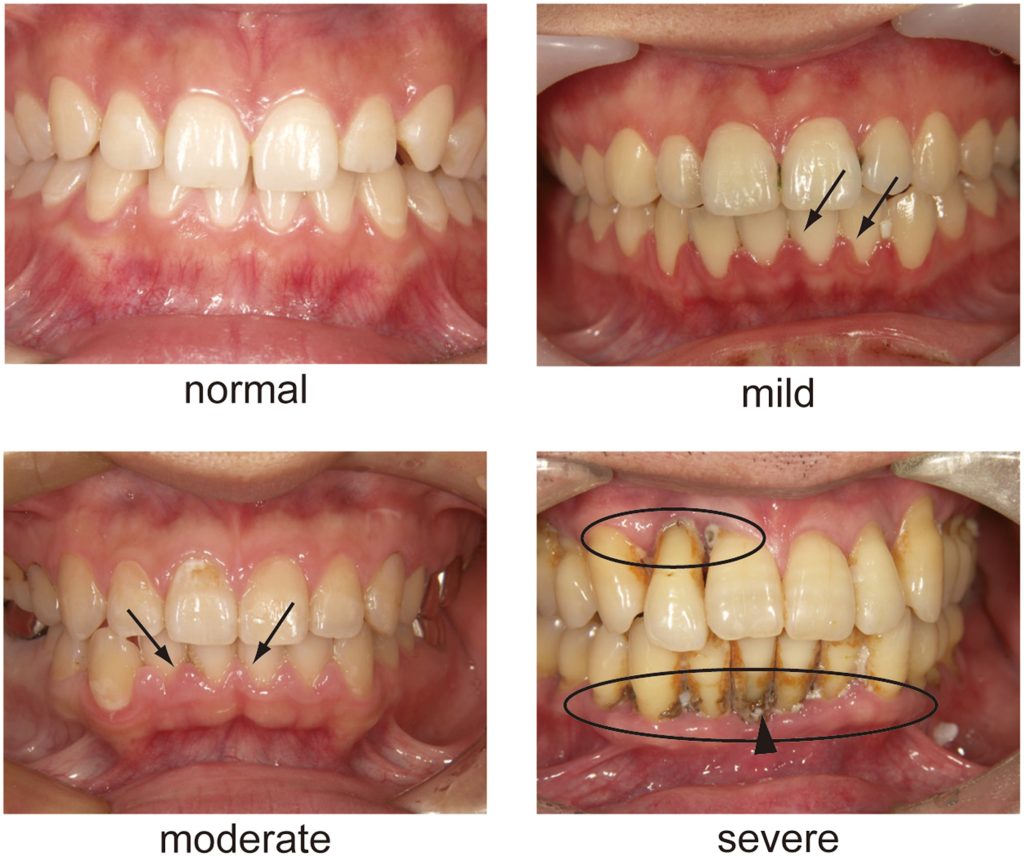
Gum recession:
Some individuals have thin gum tissue as a genetic predisposition. Periodontal disease also causes gum recession in other people. Gum recession occurs when the gum line recedes from the teeth, exposing the roots.
Gum disease:
Inflamed and painful gum tissue may result in sensitivity because the ligaments that hold the gums in place have been removed, exposing the root surface that directly connects to the tooth’s nerve.
Cracked teeth:
Broken or chipped teeth may allow plaque-containing germs to enter the pulp and cause irritation.
Grinding or clenching:
Doing this to your teeth can wear away the enamel and reveal the dentin beneath.
Products for teeth whitening:
These products are a main cause of tooth discomfort. Speak to a dentist about teeth whitening for sensitive teeth if you wish to improve your smile.
Age:
Between the ages of 25 and 30, teeth sensitivity is at its peak.
Plaque accumulation:
Root surface sensitivity may be brought on by the presence of plaque.
Use of mouthwash:
If you have exposed dentin, several over-the-counter mouthwashes include acids that might exacerbate tooth sensitivity (the middle layer of the tooth). The dentin layer of the tooth is further harmed by the acids. Consult your dentist about using a neutral fluoride solution if you experience dentin sensitivity.
Acidic foods:
Erosive enamel can result from routinely consuming foods with a high acid content, such as citrus fruits, tomatoes, pickles, and tea.
Recent dental procedures:
Following fillings, teeth cleanings, and dental restoration placement, patients may experience sensitive teeth. Dental procedure-related sensitivity is transient and often goes away in four to six weeks.
Sensitive teeth diagnosis
Make an appointment with your dentist if this is the first time you’ve noticed tooth sensitivity. You may make a dental appointment with a professional in your neighbourhood. They can examine the condition of your teeth and search for any issues that might be causing the discomfort, such as cavities, loose fillings, or receded gums.
During your regular teeth cleaning, your dentist can perform this. They’ll perform a visual inspection and clean your teeth. They might use dental tools to gently touch your teeth to check for sensitivity, and they might also request an X-ray to rule out other possibilities like cavities.
Treatment of teeth sensitivity
Your dentist can employ a variety of techniques to reduce your discomfort once the issue has been identified, including:
- toothpaste for teeth that are sensitive
- The fluoride gel
- coverings for exposed roots
- Sealants
- You can purchase desensitising pastes from your dentist (not to be used with a toothbrush).
- If you grind your teeth, wear a mouthguard.
- A root canal may be recommended by your dentist if your condition is serious.
Additionally, it’s critical to avoid avoiding dental care due to tooth pain. Ignoring your teeth can exacerbate the situation. Twice-daily brushing and flossing will maintain your smile healthy and pain-free. Additionally, go to the dentist twice a year for a checkup.
Prevention tips for sensitive teeth
People can lessen tooth sensitivity and safeguard their tooth enamel by:
- using a fluoride toothpaste to wash your teeth twice a day
- once daily flossing
- taking pauses from tooth whitening
- minimising intake of foods that are high in sugar, carbohydrates, and acids
- reducing alcohol consumption
- using a mouthguard at night to avoid clenching and grinding
- regular dental visits
- giving up smoking
REFERENCES:
- https://www.healthline.com/health/sensitive-teeth
- https://www.medicalnewstoday.com/articles/324731
- https://my.clevelandclinic.org/health/symptoms/10954-teeth-sensitivity
- https://www.webmd.com/oral-health/guide/tooth-sensitivity
For more details, kindly visit below.