A month following stent implantation, stopping aspirin may not raise the risk of blood clots.
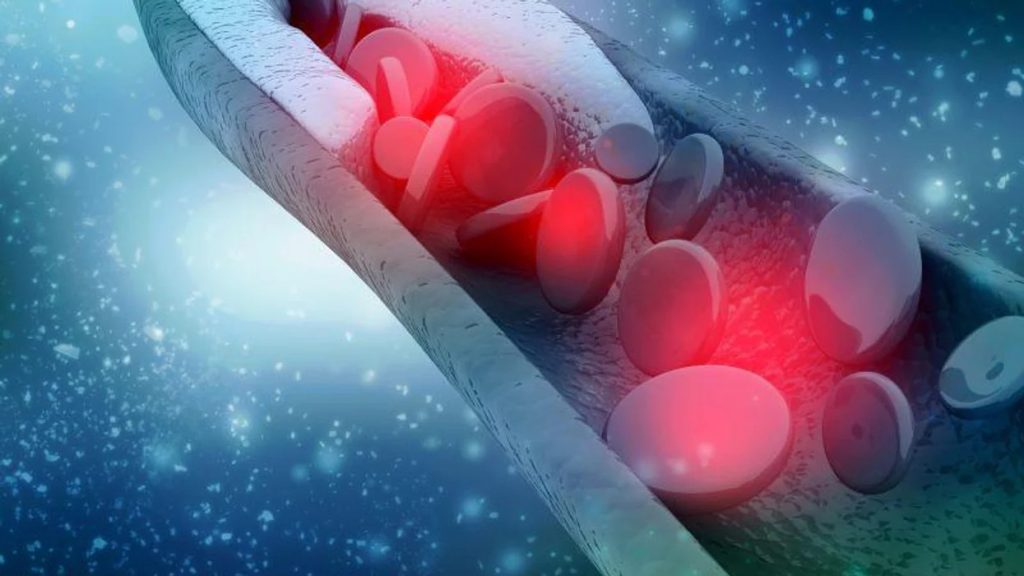
Following a percutaneous coronary intervention (PCI) to treat a heart blockage, physicians typically prescribe two antiplatelet medications or blood thinners for one year. According to a recent study, those blood thinners could be safely reduced in half in just one month. Research indicates that patients can safely stop taking one blood thinner after taking two for a month, and there is no increased risk of clots forming on the hardware implanted during percutaneous coronary intervention.
Blood thinners can cause bleeding, make it difficult for scabs to form over wounds, and cause other negative side effects, even though they provide significant protection against the formation of clots. Dual antiplatelet therapy, or DAPT, combines antiplatelet medications used after surgery. It usually contains a stronger P2Y12 receptor inhibitor (there are several), along with aspirin. The medication ticagrelor was used in the study. DAPT is recommended for a full year because there is a decreased chance of clotting beyond that time.
The research examined treatment plans and results for 3,400 Acute Coronary Syndrome patients at 58 facilities in China, Italy, Pakistan, and the U.S. K., from October 2022 to August 2018. Every research participant had undergone PCI. Once stable for a month following the procedure, they were randomized into one of two groups. The new DAPT consisted of ticagrelor and placebo for 1,700 patients. For the entire year, the remaining people took aspirin and ticagrelor.
After one month, 78 participants taking ticagrelor-aspirin experienced major or minor bleeding events, while only 35 participants in the ticagrelor-placebo group experienced such events. This equates to a 55% decrease in bleeding incidents. Significant cardiovascular events were statistically comparable in the two groups, indicating that the ticagrelor-placebo group’s stop of aspirin did not lead to a rise in unfavorable cardiovascular outcomes. There are two ways to address the issue of blocked arteries. The only procedure available to us back then was bypass surgery, in which a surgeon physically enters the body and reroutes all blood flow around the blockages.
Over the past three decades, percutaneous coronary intervention has been used. This minimally invasive technique involves threading small catheters through the groin or wrist to the heart, where doctors use wires, balloons, and stents to open up blocked arteries. Blood clots can form around these devices, which is why patients are often prescribed dual antiplatelet therapy to prevent ischemic events. Compared to bypass surgery, percutaneous coronary intervention is a much less invasive and more common procedure now.
Every hospital performs percutaneous coronary interventions daily, according to Chen. The study tackles a balancing act that has long been a source of difficulty for cardiologists. The problem was explained by Jayne Morgan, MD, a cardiologist and the Executive Director of Health and Community Education at Piedmont Healthcare Corporation in Atlanta, Georgia. She was not involved in the study. The main goal of DAPT is to prevent ischemic events, but as the risk-benefit ratio is considered, there has been some discussion about DAPT after PCI in patients with both acute and chronic coronary syndromes..
She stated it is obvious that the risk of more ischemia needs to be decreased. Morgan called the results compelling and expressed her anticipation for more data on the subject, but at what cost to increased bleeding and its inherent morbidity on the patient as well? According to her, Single Action Platelet Therapy with ticagrelor alone between months one and twelve seems to have produced a comparable rate of MACCE [major adverse cardiac and cerebrovascular events] with fewer bleeding complications.
This study answers a question that we were all curious about. Even though it’s unquestionably a safer strategy than what we’re all doing right now, it demonstrates that this approach is effective. Furthermore, it demonstrated that things weren’t worse. You were giving the two blood thinners, but it wasn’t leading to more clots forming on the stent. We really need to know that information, Chen said. He stated that things won’t change right away because the protocol of administering two blood thinners after PCI has been in place for decades. The American Heart Association, American Cardiology College, and the Society for Cardiovascular Angiography and Interventions are among the significant advisory bodies that update their recommendations yearly. Chen predicted that this would be a significant step toward future changes to these rules.
Medications that have been suggested by doctors worldwide are available here
https://mygenericpharmacy.com/index.php?cPath=741