Why dementia risk is higher for people with irregular sleep patterns
Maintaining a regular sleep schedule is just as important to your general health as getting enough sleep. According to a recent study that was published in Neurology, persons with extremely erratic sleep patterns may be more susceptible to dementia than people with more regular sleep patterns. An average of 62 years old, 88,094 people were observed by researchers over about 7 years.
A wrist device was worn by participants for a week to track their regularity and sleep cycle. The group created a score for irregular sleep patterns based on these data. After that, the researchers looked through the participants’ medical records to determine which of them had dementia. They discovered that the highest sleep irregularity was associated with a 53% higher risk of dementia development compared to moderate sleep irregularity.
According to Matthew Pase, PhD, of Monash University in Melbourne, Australia, the correlation between sporadic sleep patterns and the likelihood of developing dementia was strong, particularly considering the size of the sample. He made this observation to Healthline. Additionally, the results were unaffected by the length or disruption of sleep, indicating that regularity of sleep is significant in and of itself. Based on this data, researchers and the general public should think about sleep regularity in addition to overall sleep duration and quality when defining what constitutes good sleep.
Future research, according to study co-author Pase, could look into whether getting enough sleep enhances memory. Research may also look into the mechanisms relating regular sleep patterns to dementia. For instance, are there any connections in the brain between regular sleep patterns and Alzheimer’s disease? Pase said.
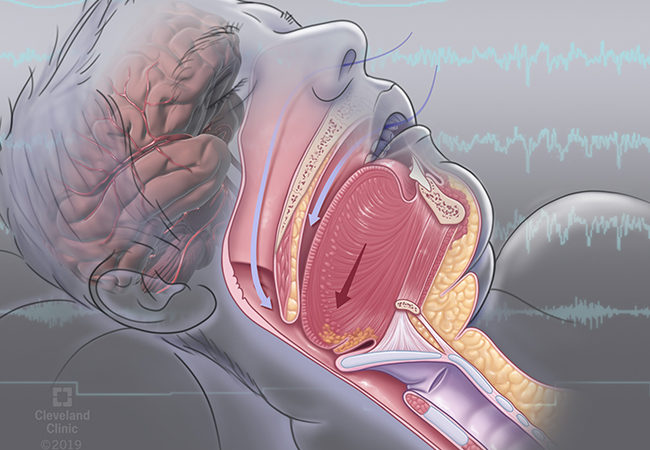
According to sleep experts, the human body naturally follows circadian rhythms, or sleep-wake cycles, which are synchronized with the time of day. A pattern of day-night oscillation of neural, hormonal, and other regulatory system patterns that respond best to environmental light is known as the circadian system. This especially applies to sunlight. According to experts, this system is impacted by irregular sleep patterns, which may also increase the risk of cognitive decline.
The circadian timing system, which runs concurrently with our sleeping and waking, is challenged by irregular sleep patterns, according to Mary A. Carskadon, Ph.D., a professor of psychiatry and human behavior at Brown University’s Warren Alpert Medical School. The circadian system receives a strong “darkness” signal from sleep, which aids in establishing and maintaining circadian timing.
According to Dr. Sudha Tallavajhula, medical director of the Neurological Sleep Medicine Center at TIRR Memorial Hermann and a sleep neurologist at UTHealth Houston, sleep is a natural human phenomenon that should be synchronized with day-night rhythms. Multiple networks collaborate to coordinate immune response, hormone production, and other vital organ system functions, all aimed at regulating the human rest-activity cycle. These networks begin with specialized cells in our eyes.
Tallavajhula did not contribute to the research. Cerebrospinal fluid has been shown in recent research to aid in the brain’s waste-removal process while you sleep. A recently identified role of sleep is the brain’s glymphatic system, which is responsible for removing waste materials from the brain, or Carskadon. It’s easy to see how a series of these actions could lead to a potentially dangerous build-up of material that, over time, could impair cognitive function. A regular schedule for going to bed and waking up is crucial for maintaining regular sleep patterns.
The US. S. The following are suggestions for improving sleep quality from the Centers for Disease Control and Prevention: Establish a regular bedtime and wake-up time. Make sure your bedroom is peaceful, cozy, and dark. Do not store electronics in your bedroom, such as a laptop, tablet, or phone. Large meals, coffee, and alcohol should be avoided right before bed. Engage in regular exercise. Regular sleep schedules are important, Tallavajhula agrees.
The most frequent action that specialists in sleep medicine recommend to enhance sleep is establishing a regular schedule, according to Tallavajhula. It’s like working out at the gym, only this is mental exercise. Some individuals may find it difficult to stick to a regular sleep and wake-up schedule, particularly shift workers.
That’s when Tallavajhula suggested avoiding rotating shifts and adopting a different sleep schedule. In contrast to those who sleep more regularly, individuals with irregular sleep patterns may be more susceptible to dementia, according to recent research. Cognitive performance is negatively impacted by irregular sleep, which disrupts the body’s circadian rhythm. Both getting enough sleep and adhering to a regular sleep schedule are crucial, according to experts.
REFERENCES:
Medications that have been suggested by doctors worldwide are available here
https://mygenericpharmacy.com/index.php?cPath=77_314