Most people with heart disease consume excessive amounts of sodium, study finds
Many people, especially those who should limit their intake due to heart health concerns, consume more sodium than is advised daily. This is supported by a recent study that discovered individuals with cardiovascular disease (CVD) were ingesting more than twice as much sodium per day 1,500 mg—as is advised. The study participants consumed an average of 3,096 mg of sodium daily, with 89% consuming more than the recommended amount. The results will be presented from April 6–8 at the Annual Scientific Session of the American College of Cardiology. The findings are still pending publication in a peer-reviewed journal.
The American Heart Association (AHA) advises adults without a history of heart disease or those not suspected of being at risk to consume no more than 2,300 mg of sodium daily. This is roughly the same as one teaspoon of table salt. This study’s average heart disease patient was over 1,000 mg above that threshold. 3,170 participants in the NHANES study conducted by the Centers for Disease Control provided data for the study. Men and women with a diagnosis of cardiovascular disease who were older than 20 were included in this sample. White people 65 years of age or older with less education than a high school diploma made up the bulk of this group. With an average daily calorie intake of 1,862, males, who made up slightly more than half of the subjects (56.4%), were overweight. Although it’s commonly believed that having fewer food options leads to excessive sodium consumption, this study challenges that theory.
Those with a college degree or above and those at the higher end of the income spectrum consumed the most sodium. The unexpected findings may have been influenced by the fact that people with greater incomes and educational backgrounds may have been more accurate in disclosing their sodium consumption, according to the study’s authors. Sodium chloride is the chemical name for table salt. In trace amounts, sodium, a naturally occurring mineral, is essential to human health. According to cardiologist Jayne Morgan, MD, clinical director at Piedmont Healthcare Corporation in Atlanta, GA, sodium helps to balance the water in your body. It even helps to maintain the healthy operation of nerves and muscles.
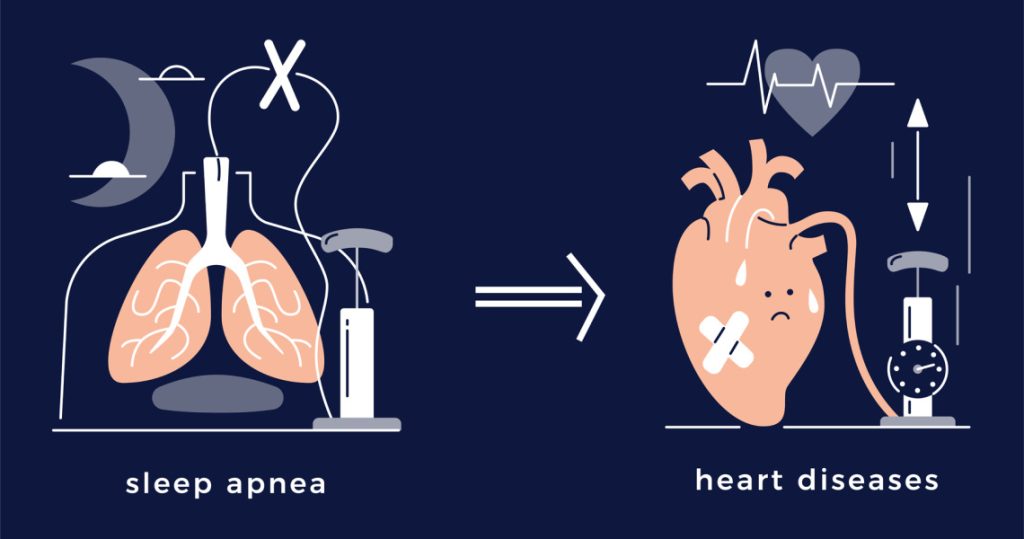
Your body’s blood volume rises as a result of salt. High blood pressure is the result of this. Due to the increased cardiac workload caused by the elevated blood pressure, you may eventually develop heart disease. Atherosclerosis and the hardening and stiffening of the arteries have long been associated with excess sodium, according to Dr. Morgan. Numerous studies have examined the reasons behind the widespread desire for salt.
According to registered dietitian nutritionist Michelle Routhenstein, MNT, “the consistent overconsumption of sodium across the socioeconomic spectrum suggests that factors beyond just access to resources may influence sodium intake.”. Routhenstein did not work on the project. According to Routhenstein, this might imply the marketing and general availability of processed foods that are easily accessed and high in sodium, cultural eating habits that value salty foods, and a lack of knowledge or instruction regarding the health risks connected to consuming excessive amounts of sodium.
This is a powerful illustration of how common the Western diet is and how much people crave salt and “flavor.”. It also illustrates how simple and readily available sodium is in a lot of grocery items, even when purchasing ‘healthy’ alternatives. According to her, the Food and Drug Administration (FDA) could establish a uniform food rating system that would enable everyone to know where a given food choice falls on a health spectrum. At that point, the customer can make an informed choice. The first step in lowering sodium consumption is to monitor your salt intake, but it can be challenging to determine how much sodium you’re really taking in.
Sodium is used in many food products for purposes other than just adding flavor. It has multiple uses, including baking, thickening, curing meat, retaining moisture, and serving as a preservative. A lot of sodium-rich foods don’t even taste salty. According to Routhenstein, people may unintentionally consume excessive amounts of sodium if they don’t actively read food labels and pay attention to sodium levels. Before even thinking about using a salt shaker, people might not be aware of how much sodium is in their food, according to Routhenstein. For instance, the recommended sodium intake for people with heart disease can be exceeded by the 2,000 mg or more found in a typical restaurant meal.
Using fresh ingredients when cooking at home, selecting low-sodium options, incorporating herbs and spices for flavor, reading labels, and being aware of hidden sodium in processed foods are all good ways to reduce your intake of sodium through diet. While eating out, people can choose heart-healthier, lower-sodium options by asking for dressings and sauces to be served on the side, choosing grilled or steamed food over fried, and asking for meals to be prepared without added salt. While [you’re] still enjoying delicious meals, these small changes can make a big difference in your overall sodium intake reduction. Routhenstein offered a variety of flavor-retaining salt substitutes, such as a small amount of lemon or grapefruit juice added to recipes.
Citrus fruits’ tart flavor can fool the palate into thinking food has more salt than it actually does, keeping food tasty even when it contains less sodium. Furthermore, Routhenstein promoted spiciness; add hot sauce or chili peppers to your food based on your personal preferences. You could also use a shaker of your favorite powder, like oregano or garlic powder, in place of the tabletop salt shaker (not garlic salt, which contains sodium). Seasonings such as Dijon mustard, whole grain mustard, or dry mustard powder can give dressings, marinades, and sauces tang and depth. According to Routhenstein, adding mustard to rubs, sandwich spreads, and vinaigrettes provides a tasty variation without using a lot of sodium.
Medications that have been suggested by doctors worldwide are available here
https://mygenericpharmacy.com/index.php?cPath=77_99