Is placebo just as good as opioids for lower back?
For the treatment of neck pain and low back pain, researchers examined the effectiveness of opioids with a placebo. After six weeks of therapy, there were no appreciable differences in pain scores between the opioids group and the placebo group. After a year later, the placebo group had somewhat lower pain scores.
The results imply that opioids might not be successful in treating some types of pain.
The greatest cause of disability worldwide is lower back pain. 619 million people worldwide would be impacted by the illness in 2020. This number is projected to rise to 843 million by 2050.

According to estimates of “years lived with disability,” neck discomfort is the fourth most common cause of impairment globally and a major contributor to disability.
When alternative treatments have failed to relieve a person’s lower back or neck pain, clinical guidelines advise turning to opioid medicines. According to studies, many people with the disorders, including two-thirds of those in Australia, may first try opioids.
Despite this, there isn’t much proof that opioids work well for treating neck and lower back pain. It is also well known that using opioids as a treatment raises the chance of unfavourable outcomes like opioid dependence, abuse, and overdose.
Treatment options may be influenced by additional research on the effectiveness of opioids in treating lower back and neck pain.
Researchers from the University of Sydney in Australia recently looked into the effectiveness and safety of brief opioid treatment regimens for treating neck and lower back pain.
They discovered that the risk of abuse rose with subsequent opioid treatments and that opioids did not provide better pain relief than a placebo.
There is no discernible difference between opioids and a placebo.
The average age of the 347 people the researchers enrolled in the study was 44,7. Nearly half of the participants were female, and all had experienced lower back pain, neck pain, or both for 12 weeks or less.
The patients were divided into two groups at random and either received the indicated treatment plus the opioid oxycodone-naloxone or the recommended treatment plus a matching placebo for up to six weeks.
Care that was advised by guidelines included assurance and suggestions to be active. Participants could seek additional care if needed after six weeks.
There was no discernible change in pain levels between the opioid and placebo groups, after 6 weeks of treatment. After accounting for the location of the pain and the number of days after the pain started, the results remained unchanged.
After 12 weeks, there was little difference in the pain scores between the placebo and opioid groups, but by week 52, individuals in the placebo group had slightly lower pain scores.
At week 6, the opioids and placebo groups’ average pain scores were 2.78 and 2.25, respectively. At 52 weeks, the opioids group’s pain score was 2.37, compared to 1.81 for the placebo group.
They also discovered that there was no difference in the groups’ physical quality of life. At 6 and 12 weeks, however, the placebo group’s mental health showed a modest but substantial improvement.
The number of participants reporting adverse events was the same in both groups, but the opioid group was more likely to develop opioid misuse.
On the Current Opioid Misuse Measure Scale, 20% of the opioid group and 10% of the placebo group were categorized as “at risk” after 52 weeks.
Why don’t opioids work?
Dr. Wang Lushun is a senior consultant orthopedic surgeon at Arete Ortho in Singapore and a non-participant in the study. He was questioned about the potential ineffectiveness of opioids for treating lower back and neck pain.
Opioids are typically used to treat pain, but recent research suggests that they might not be as beneficial for neck and lower back pain. This is because opioids primarily target pain perceptions rather than the underlying causes of pain, according to Dr. Wang.
“The medications aid in reducing pain perception by attaching to opioid receptors in the brain. However, the main causes of these pains inflammation or physical harm are not actually relieved,” he said.
“The body can get tolerant to opioids over time, necessitating the use of greater doses to provide the same amount of pain relief”. Dr. Wang Lushun warned that this could result in adverse effects and perhaps reliance. One such side effect is a condition known as opioid-induced hyperalgesia, which can make pain worse.
What are the research’s constraints?
Dr. Joel Frank is a licensed psychologist at Duality Psychological Services in California who was not engaged in the study. He responded to our inquiry regarding the study’s shortcomings:
“First off, although 42% of the sample failed to follow the treatment strategy, which was medication-focused. Second, they claimed that the care was “not monitored,” even though their “guideline care” recommended physical activity.
Thirdly, Dr. Frank noted that the BPI, a self-report measure, was used as their main indicator of pain intensity. Self-report assessments are by nature subjective. To obtain a more complete picture of the subjective experienced pain Lee patients, it is recommended to integrate extra measures that assess pain catastrophization when using self-report measures for pain.
Additionally, we had a conversation with Dr. Vernon Williams, a sports neurologist, pain management expert, and founding leader of the Centre for Sports Neurology and Pain Medicine at Cedars-Sinai Kerlan-Jobe Institute in California who was not affiliated with the study.
“Your body’s reaction to the anticipation of the active treatment and your body’s reaction to the possible benefit or anticipation of the placebo both have physiological effects. The study revealed that the opioid did not perform better than the placebo, not that it was ineffective. It’s a small but important difference,” he said.
A senior research scholar at the University of Sydney in Australia who was not involved in the study, Dr. Gustavo De Carvalho Machado, was also questioned about its shortcomings. He issued the following advice:
The results do not necessarily apply to emergency rooms and pre-hospital situations, where patients need an ambulance. The outcomes of this research were examined weeks after recruitment, and in emergency settings, prompt analgesia within hours is critical for management and discharge planning. Patients who present to these settings have more severe pain and disability.
Alternatives to traditional medicine for back pain
De Mesa was also asked about possible treatments for neck and lower back problems.
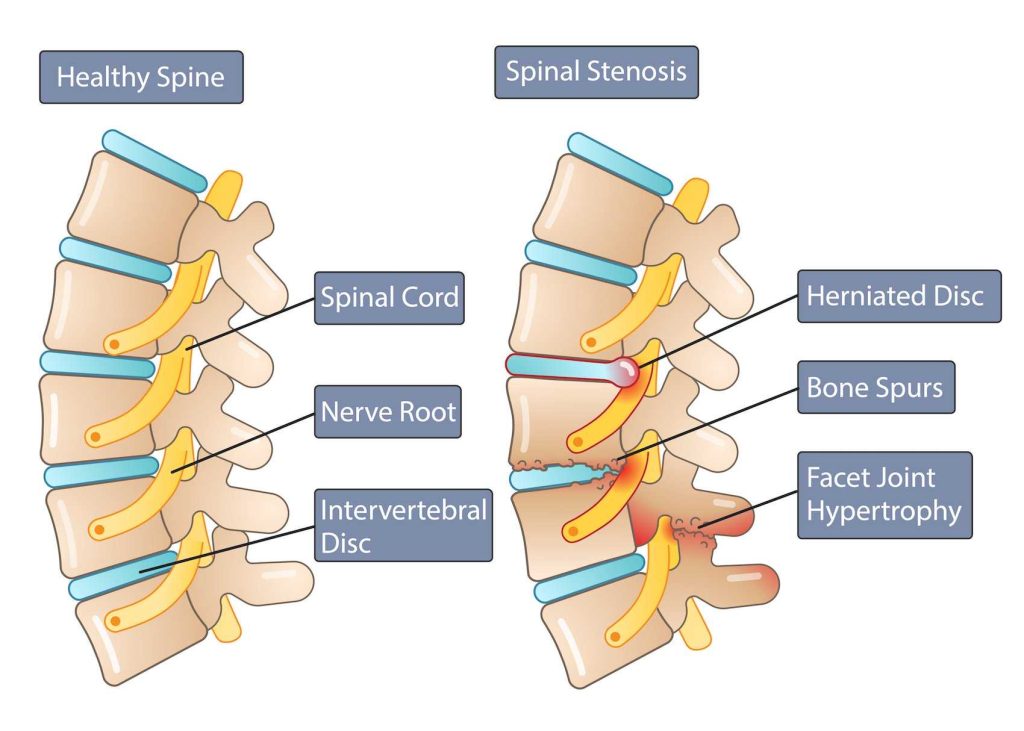
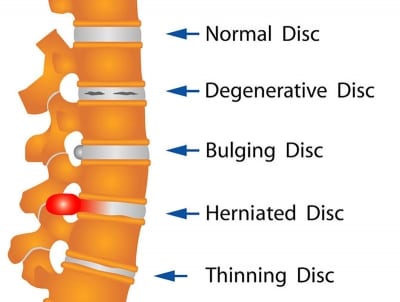
“More efficient solutions for neck and lower back pain deal with the underlying problems. For instance, a doctor can assist in identifying the precise muscles and/or surrounding tissues, such as tendons and ligaments, that are involved. Exercise, better ergonomics, and physical treatment may be advised,” he said.
Since spinal pain frequently has multiple causes, a holistic approach to treatment can aid in the patient’s long-term healing. Acupuncture, diet, cognitive behavioral therapy, and educational programs are all helpful in addition to physical fitness. As required, over-the-counter anti-inflammatory drugs can be taken. Depending on the needs and circumstances of the individual, the optimum treatment strategy will change, he said.
De Mesa stated that spine surgeons, pain specialists, and board-certified physiatrists may be suggested for chronic spinal pain.
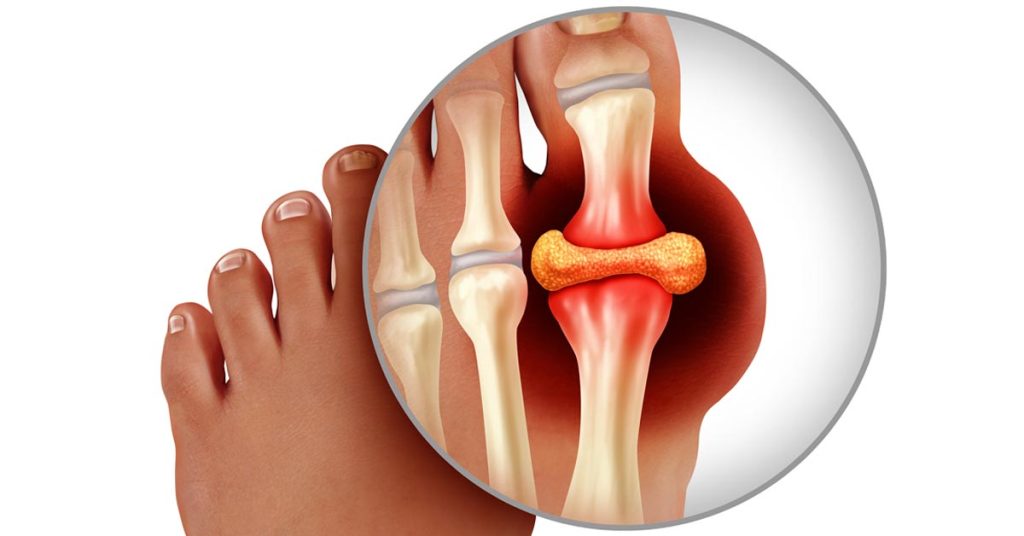
“Arthritis of the spinal joints or inflammation of the vertebral endplates may be the source of chronic pain. It may be advised to administer injections to locate the source of the pain and treat it,” the doctor said.
“Basivertebral nerve ablation and radiofrequency ablation of the spinal medial branch nerves are two examples of interventional therapies that may lessen pain and enhance quality of life. Surgery is only used as a last resort and is only done when it is judged medically essential,” he added.
REFERENCES:
- https://www.medicalnewstoday.com/articles/opioids-about-as-effective-as-placebo-for-lower-back-and-neck-pain-study-finds
- https://pubmed.ncbi.nlm.nih.gov/23983011/
- https://www.npr.org/sections/health-shots/2023/06/28/1184885112/back-pain-relief-opioid-painkillers
For Bone disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=63