Air pollutant may increases asthma attack in urban children
Viral respiratory infections are a typical cause of asthma attacks. Thisinvolve a worsening of the inflammation and a narrowing of the bronchial airways. Nevertheless, non-viral causes of asthma attacks are also possible.
Asthma attacks are more likely to occur when people are exposed to more air pollutants. However, the molecular mechanisms by which air pollutants might cause asthma attacks are poorly understood.

A recent study found that children living in metropolitan areas were more likely to experience asthma attacks. Due to exposure to greater levels of air pollutants, specifically ozone and fine particle matter. The most frequent cause of asthma attacks is viral respiratory infections. However nonviral variables including air pollution can also contribute to an asthma attack’s onset.
According to a recent study, children who live in urban areas are more likely to experience asthma episodes. Also, their lung function declines when air pollution levels are higher. Particularly when ozone and fine particulate matter concentrations are high.
Researchers found that these air pollutants could cause asthma attacks. Even when their concentrations were below the threshold set by the federal government for air quality.
The researchers also found that elevated ozone and fine particulate matter were linked to particular inflammatory pathways in the airways. Providing further insight into how elevated levels of pollutants may raise the likelihood of asthma episodes in urban children.
Asthma attacks: What to know
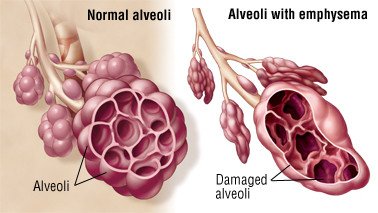
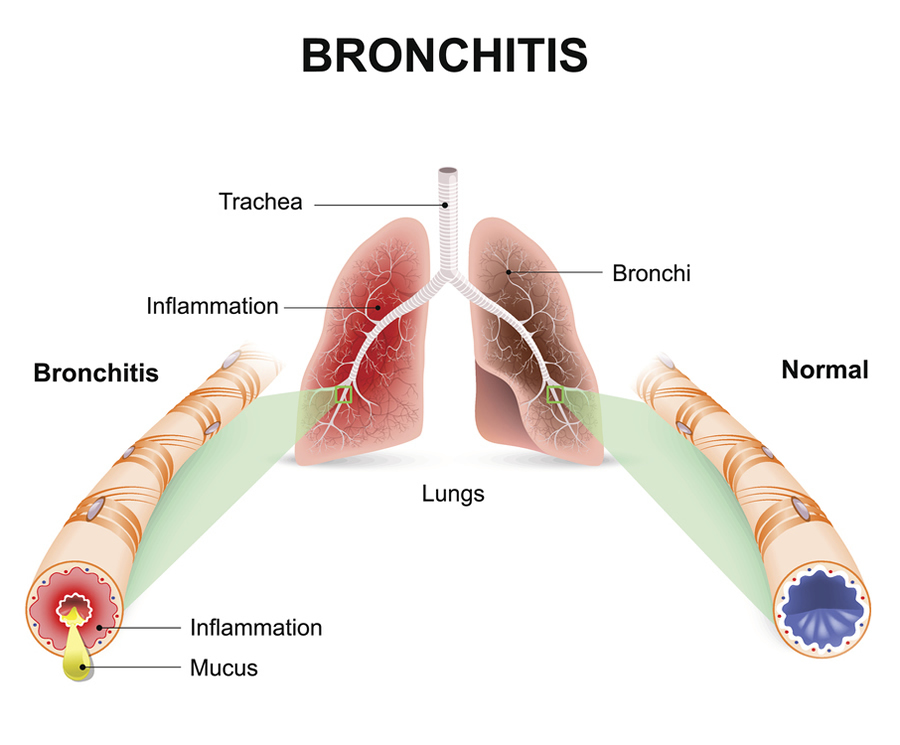
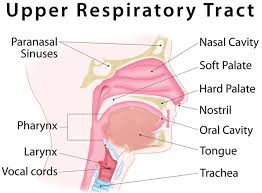
The primary airways in the lungs, the bronchi, and their branching, become inflamed and constricted in people with asthma. Chest constriction, shortness of breath, coughing, and wheezing are among asthmatic symptoms. They tend to get worse while the condition is exacerbating.
The lung airways are further constricted during an asthma exacerbation. Sometimes referred to as an asthma attack, as a result of the airway cells’ inflammation and the bronchial muscles’ spasm. Moreover, there is an increase in mucus production at the same time, which obstructs the airways.
One of the most frequent reasons for asthma flare-ups in both children and adults is respiratory tract viral infections. However, non-viral factors including allergens, pollen, and pet hair, as well as non-viral diseases, can also contribute to an asthma exacerbation.
Also, a number of epidemiological studies have linked the frequency of asthma attacks and air pollution levels. Asthma attacks have been connected to higher concentrations of a number of air pollutants. This including fine particulate matter, ozone, nitrogen dioxide, and sulphur dioxide.
One of the most prevalent chronic diseases in children is asthma. Also, research indicates that children who live in low socioeconomic and urban neighbourhoods have greater asthma prevalence and morbidity rates. These communities typically have higher air pollution levels. This may help to explain why asthma is more common and severe in children living in low-income metropolitan regions.
Yet, particularly in sensitive populations like children with severe asthma, the molecular pathways behind asthma exacerbation during non-viral respiratory infections are poorly known. Also, the variations in the mechanisms behind asthma flare-ups brought on by viral infections and airborne contaminants have not been defined.
Impact of air pollutants on asthma
In the current study, the researchers first looked at the relationship between air pollution levels and asthma flare-ups in kids and teenagers living in metropolitan areas. Data from an earlier observational trial titled “Mechanisms Behind Asthma Exacerbations Prevented and Sustained with Immune-based Treatment Part 1” was analysed by the researchers.
The current study’s objective was to particularly comprehend the molecular basis of non-viral asthma exacerbations brought on by air pollution using the MUPPITS1 data.
208 children with asthma who were prone to exacerbations and lived in low-income areas of nine American cities were enrolled in the MUPPITS1 study. Following the onset of respiratory illness symptoms in these subjects, the study took measurements of lung function and nose swabs.
The nasal samples were utilised by the researchers to identify whether non-viral or viral infections were to blame for the respiratory ailment. They further divided the subjects into groups according to whether or not an asthma exacerbation occurred when they were unwell.
The Environmental Protection Agency (EPA) collected data on specific pollutant concentrations and the Air Quality Index for each study region. The researchers then used this information.
The researchers reported that the Air Quality Index values were higher nine days before and after the beginning of symptoms in participants with a non-viral asthma exacerbation than those with a viral asthma exacerbation. The participants who had non-viral asthma exacerbations also showed a negative correlation between the Air Quality Index values and lung function.
Profile of gene expression
The nasal samples from the MUPPITS1 investigation were then used by the researchers to analyse variations in gene expression.
In both viral and non-viral asthma exacerbations, the Air Quality Index was associated with common gene expression patterns. Pointing to the existence of fundamental processes underlying asthma attacks. Moreover, changes in the gene expression profile that were unique to non-viral asthma exacerbations were linked to Air Quality Index levels.
It was found that fine particulate matter concentrations were directly correlated with an increase in genes. It is linked to excessive mucus secretion and proinflammatory cytokines, a class of signalling proteins, in non-viral asthma exacerbations.
The expression of tissue kallikreins, a class of enzymes involved in inflammation and increased in asthma, was positively linked with fine particulate matter concentrations.
The majority of the respiratory tract is lined by epithelial cells. They shield the respiratory system from allergens, pathogenic agents, and debris that can injure it when inhaled. The expression of genes related to epithelial cell barrier function was also correlated with the amounts of fine particulate matte
According to researchers, the greater asthma prevalence and morbidity in children living in urban centres may be explained. Due to the molecular pathways implicated in asthma exacerbations linked to certain air contaminants.
Identifying the molecular pathways that are unique to asthma flare-ups brought on by increased levels of air pollution may potentially aid in the development of therapies that target these pathways.
Moreover, using air filters during periods of high air pollution and using personal air quality monitoring equipment may help reduce the risk of asthma flare-ups related to air pollution. The study was observational in nature, and the authors noted that it did not prove a connection between air pollution and the frequency of asthma attacks.
Facts
To better prevent and treat asthma in these patients, it is concluded that more research is required to understand the underlying processes of the connection.
Although initiatives like selective planting around school playgrounds could help limit exposure among this vulnerable demographic, air pollution in underdeveloped areas has also been linked to impaired cognitive capacities in youngsters.
REFERENCES:
- https://www.medicalnewstoday.com/articles/nih-study-links-specific-outdoor-air-pollutants-to-asthma-attacks-in-urban-children
- https://www.ajmc.com/view/specific-air-pollutants-linked-to-asthma-attacks-in-urban-children
- https://www.earth.com/news/specific-air-pollutants-linked-to-asthma-attacks-in-urban-children/
- https://www.usnews.com/news/health-news/articles/2023-01-06/polluted-air-means-more-asthma-attacks-for-urban-kids
For more details, kindly visit below.