According to research, eating more fruits and vegetables reduces the chance of death in persons with chronic renal disease.
Doctors may recommend a low-potassium diet to patients with severe chronic kidney disease (CKD) because their kidneys have trouble processing it, resulting in excessive potassium levels in the blood.
In this study, researchers discovered comparable baseline serum potassium levels stratified by CKD stage in various groups based on how frequently they consumed fruits and vegetables.
According to the researchers, this shows that regularly consuming fruits and vegetables may not be linked to a rise in serum potassium levels.
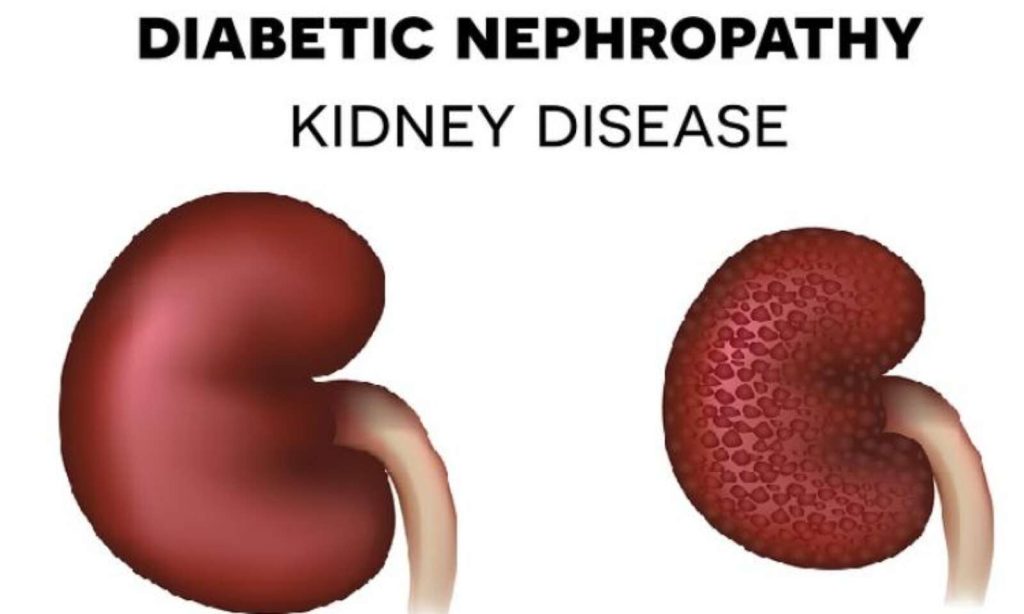
Chronic kidney disease (CKD) patients have a progressive loss of renal function. The National Institute of Diabetes and Digestive and Kidney Diseases estimates that more than one in seven persons in the United States have CKD.
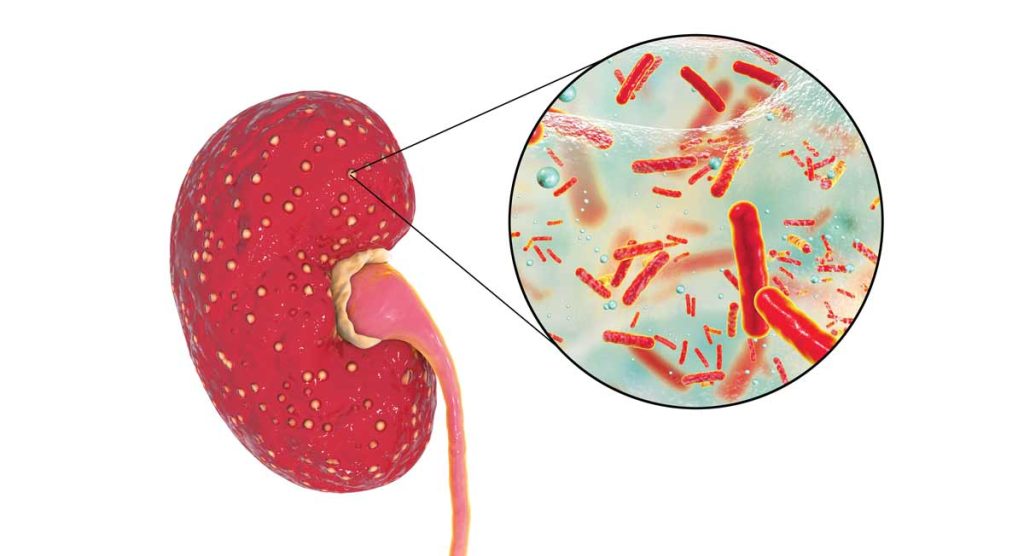
Since there are sometimes no symptoms in the condition’s early stages, CKD frequently stays undiagnosed until it is severe. Sometimes damaged kidneys cause blood levels of potassium to rise. The word for elevated potassium levels is hyperkalemia.
Researchers from one study discovered that more than half of the individuals, all of whom had severe CKD, had potassium levels above the recommended threshold. Occasionally, doctors advise patients with CKD to keep to low-potassium diets as their renal function declines.
Consuming more fruits and vegetables
Officials in charge of public health frequently extol the virtues of eating plants. Consuming fruits and vegetables has been linked to a lower risk of cancer, heart disease, and all-cause death.
According to the researchers, advanced CKD patients occasionally find themselves eating fewer meals that include vegetables and fruits due to worries about maintaining a diet low in potassium.
The 2019 systematic review of observational studies piqued the researchers’ interest because it revealed that hemodialysis patients had poor fruit and vegetable intake and that increasing consumption was linked to a lower risk of all-cause and non-cardiovascular death.
More specifically, the researchers found that consuming roughly 17 servings of vegetables and fruits each week, as opposed to just two, was related to a 20% decreased risk of all-cause mortality.
The researchers chose a Japanese hospital to carry out their study of patients with and without CKD because Asian diets are frequently higher in fruits and vegetables.
Kidney disease diet study
More than 2,000 persons 20 years or older who attended one of the hospital’s several outpatient clinics on Sado Island, Japan, between 2008 and 2016 were a part of this study.
Participants had to provide information about their intake of vegetables and fruits, as well as a record of their baseline serum creatinine and urinalysis measurements. At least one follow-up evaluation was also conducted for them.
The participants’ average age was 69. 64% of the subjects had high blood pressure, 64% were men, and 39% had diabetes.
Participants were divided into groups based on their responses to the question of how often they consume fruits and vegetables: “never or rarely,” “sometimes,” or “every day.” 15% of participants said they never ate fruits and vegetables, while about half said they did so daily.
These participants were separated into three groups: hemodialysis patients, CKD patients, and CKD patients who were not reliant on dialysis. Among the participants, 45% of the patients had CKD but weren’t dependent on dialysis, and 7% were receiving hemodialysis.
With regard to non-dialysis-dependent CKD, more than half of the participants said they regularly ate fruits and vegetables. The percentage of hemodialysis patients who reported eating fruits and vegetables every day was only 28%.
There were 561 fatalities recorded over a median follow-up of 5.7 years. Using obituaries, medical data, and reports from family or friends, researchers were able to determine whether or not the study participants had passed away.
Researchers updated the analyses to account for variables like gender and age, demographics (including individuals’ smoking status and BMI), and a variety of co-morbidities.
Survival benefit of high fruit and vegetable consumption
Those who just occasionally ate fruits and vegetables had a 25% higher chance of passing away from any cause than those who regularly consumed these meals.
A 60% increased chance of passing away from any cause existed for people who either never or infrequently ate fruits and vegetables.
According to initial findings, all CKD stage-strategy groups for vegetable and fruit eating frequency had equal serum potassium levels. This shows, according to the researchers’ article, “that frequency of vegetable and fruit intake is not associated with serum potassium levels even in patients with advanced CKD.”
According to the researchers, “the association was similar regardless of CKD status”, with no effect modification by CKD status.
Our findings imply that daily consumption of fruits and vegetables may not be related with elevated serum potassium levels and that it may actually decrease all-cause mortality in CKD patients, including those receiving [hemodialysis], as opposed to increasing it.
The researchers issued a warning in their publication that participants with severe CKD might have eaten fruits and vegetables that were lower in potassium or soaked or boiled items before eating them to eliminate potassium — a common prescription provided to Japanese CKD patients.
To the contrary, they said, “accumulating evidence suggests that dietary potassium levels are not associated with serum potassium levels or hyperkalemia.”
Kidney disease and potassium
Professor and clinical chief of nephrology at the University of California, Los Angeles’ David Geffen School of Medicine, Dr. Anjay Rastogi, told that the study was “thought-provoking” but that it had certain limitations.
He noted that compared to Americans, a large portion of the population in Japan consumes more fruits and vegetables.
Rastogi was concerned that the individuals would have only submitted labs from one date and had only once reported on their consumption of fruits and vegetables. There were many details that were missing, he claimed.
Rastogi asserted that he believes those with advanced CKD should consume a diet low in potassium. “It’s a very important mineral element in our body, but obviously in patients with kidney disease who have hyperkalemia, it can wreak havoc,” said Dr. Rastogi of potassium. “It might result in cardiac arrest.”
In order to minimise their potassium intake and keep consuming fruits and vegetables, Rastogi advised persons with CKD to engage with a trained dietitian.
There are new potassium binders on the market to treat hyperkalemia for those who cannot control their potassium through diet, he added.
Rastogi declared, “I am a very big advocate of diet and lifestyle changes for slowing down the progression of not just kidney disease but also cardiovascular disease.” Cardiovascular disease is the leading cause of death in patients with kidney disease. Both of them are interrelated.
More complex suggestions
Health professionals frequently “advise people with chronic kidney disease in ways that are not very nuanced,” according to Dr. Deidra Crews, a professor of medicine in the division of nephrology at the Johns Hopkins University School of Medicine in Maryland.
Diets heavy in potassium may be problematic for some people who have very severe chronic renal disease, or even kidney failure, she explained. “However, the vast majority of individuals with chronic kidney disease really have less severe forms of the condition.
Therefore, the majority of the more than 37 million Americans with chronic kidney disease have this type of less severe disease, and the dietary practises that will help them avoid cardiovascular disease and live [a long life] will be very similar to what we might suggest to the more general population, which is: eat your fruits and vegetables.
According to Crews, study into whether diets high in fruits and vegetables are genuinely linked to hyperkalemia in persons with severe CKD is sparked by studies like this one out of Japan.
Even though individuals with advanced CKD frequently cannot eliminate potassium from their bodies through the kidneys, they may be able to do it through “pathways that exist in the gut, in the bowels,” the expert noted.
Crews emphasised that because fruits and vegetables frequently have significant fibre content, they might aid in the process.
REFERENCES:
For Chronic Kidney Disease disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=82