In the United States, more than 40% of adults are obese, with approximately 10% having extreme obesity.
Obesity increases the chance of developing a variety of ailments, such as type 2 diabetes, heart disease, and several malignancies.
An energy imbalance between calories consumed and calories burned is the primary cause of obesity.
Obesity, however, may result from more than just calorie intake—it may also result from the calories.
According to recent studies, the simple sugar fructose, which is present in many foods, may be the cause of obesity and other related health issues.
Around 13% of persons globally, according to the World Health Organisation (WHO), are obese. Although obesity rates are rising in low-income nations, the majority are in wealthy nations.
According to National Institutes of Health (NIH) data, 42.4% of adults and 19.3% of children and adolescents in the United States were obese in 2017–18. Additionally, these figures are rising.
Obesity raises the risk of a number of illnesses. It is linked to a poor diet and an unbalanced energy intake, but it may also have a genetic component. These are listed by the NIH as follows:
What connection exists between fructose and obesity?
According to recent study, obesity may not just be caused by an energy imbalance; rather, the source of that energy may be what causes the illness.
According to the study, which was published in Philosophical Transactions of the Royal Society B, fructose may be the cause of obesity because of an evolutionary “survival switch” that makes people store energy from fructose rather than utilize it.
The study’s results were discussed by Dr. Eamon Laird, a postdoctoral research fellow at the University of Limerick in Ireland who was not engaged in the study, he observed:
This is a highly intriguing theory, even though it is only a narrative overview and not a systematic meta-analysis of the available data. It is conceivable that our present energy-dense diets have altered an evolutionary pathway that was advantageous millions of years ago.
Fructose converts to energy reserves.
According to the study, metabolic diseases like obesity may have arisen as a result of overstimulation of an evolutionary-based biological reaction called the “survival switch,” which is meant to safeguard animals before a crisis like hibernation.
Contrary to glucose, which is used as immediate fuel, the researchers contend that fructose causes the body to conserve energy.
This is better for an animal going into long-term hibernation than for a person who has constant access to high-sugar diets.
This “survival switch” may be more detrimental than beneficial in areas where people have easy access to food. People develop fat reserves as a result of the constant availability of high-fructose foods, which causes obesity and related health issues.
Metabolic effects of fructose
What causes fructose to make the body store energy rather than use it?
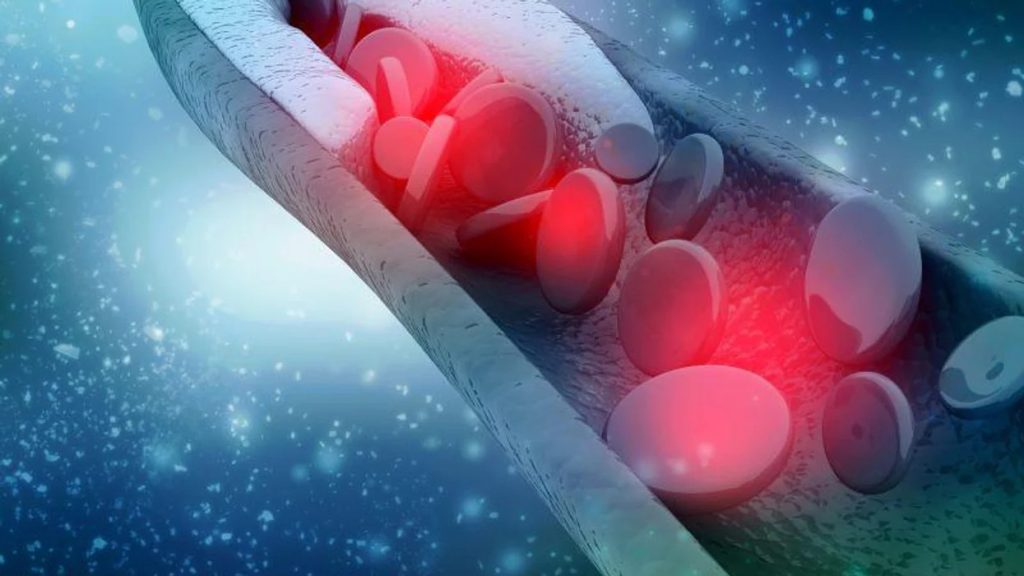
Adenosine triphosphate, or ATP, is often utilised and swiftly replaced from nutritional intake or fat storage. ATP is the chemical that supplies energy to power all cell operations.
Fructose, on the other hand, lowers the amount of ATP present in cells and hinders the production of ATP.
A chain of chemical processes that stop the mitochondria of the cell from making more ATP and put them under oxidative stress are triggered when ATP levels fall low enough.
Fructose consumption increases appetite in addition to lowering ATP levels. Once deposited as fat, these extra calories. The ATP levels eventually rise once more, but the fat reserves are still there.
Repeated exposure to oxidative stress causes mitochondrial dysfunction to become persistent over time. The body of a mammal that is hibernating adjusts to the low ATP levels by lowering the resting metabolic rate.
Without reducing calorie consumption, this lower energy usage leads to weight increase in persons who still have access to plenty of food.
Dr. Laird concurred that this theory could help to explain the rise in obesity.
He said, “I agree it could be one component. But obesity and metabolic syndrome are complex conditions; there is seldom just one contributing cause. Lack of exercise, unhealthy eating habits, vitamin deficiencies, socioeconomic causes, and even risk factors related to one’s race and ethnicity are all significant risk factors.”
Therefore, even if fructose did affect obesity, it would only have a minor impact overall, he continued.
Dietary sources of fructose
Although fruit naturally includes fructose, which gives it its sweetness, a normal Western diet also contains a variety of additional sources of fructose.
The majority comes from table sugar, high fructose corn syrup (HFCS), a sweetener manufactured from cornflour, and sucrose, a molecule composed of glucose and fructose chemically bound together.
Fructose can make up to 55% of HFCS. To transform the glucose in corn syrup into the sweeter-tasting fructose, manufacturers must add enzymes.
Since the fructose in HFCS is present as free molecules, it is absorbed more quickly than it is in table sugar.
HFCS is included in practically all processed foods and many other foods. They consist of:
- sodas
- fruit juices with added sugar
- crackers
- ready-made meals
- salad dressings and condiments
- a few pastries and bread.
According to the scientists, the growth in sugar consumption, particularly that found in processed foods, fructose-sweetened beverages, and carbohydrates with a high glycemic index (GI), is related to the global epidemics of obesity and diabetes.
Must you stay away from foods high in fructose?
Although he was not involved in the study, Dr. Mir Ali, a bariatric surgeon and medical director of the MemorialCare Surgical Weight Loss Centre at Orange Coast Medical Centre in Fountain Valley, California, stated that for people who are overweight or obese, “any source of sugar, including non-processed sugars, such as those found in fruits, can have a similar effect on the body.”
“We advise our patients to minimize all sources of sugar, including fruits,” the doctor added.
However, Dr. Laird cautioned that most people should not worry excessively about fruit’s sugar content: Most of us don’t consume enough fruits, despite the fact that doing so would benefit our overall health by providing fibre, vitamins, and minerals. The modest amounts of fruit we do consume would probably not amount to much.
However, he continued, “The main risk probably arises when the fructose is highly concentrated and added to other foods (these foods often contain high fat, high sugar, and low nutrition), which could result in an increased risk of obesity.”
So maybe avoid that processed snack since it’s probably laden with fructose to help lower your risk of becoming obese.
REFERENCES:
For Type 2 Diabetes medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=20