The role of the mind in erection and erectile dysfunction.
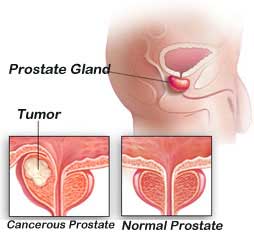
The medical problem known as erectile dysfunction (ED) is complicated and has both physical and psychological aspects. Over the past 50 years, the paradigm of what causes ED and how it is treated has moved from a mental focus to a physical one.
The development of non-invasive oral medicines and a deeper understanding of the physical aspects of ED have both contributed to this. Nevertheless, the psychological aspects of erections and ED continue to be crucial, although sometimes going unnoticed, and many men can overcome ED by addressing these elements.
While some erections appear to “simply happen,” many necessitate mental stimulation or sexual interest. Some men continue to engage in this process subconsciously, which means they do not need to actively think about sex but rather have an open mind that is susceptible to subconscious thoughts or stimuli. This is why many men don’t consider the mind’s function in the erection process until an ED develops.
Psychogenic Erectile dysfunction
The symptoms of erectile dysfunction are distinct from those of many other illnesses. Some physical conditions may have psychosomatic roots. In other words, a person’s thoughts may truly be the root of their physical ailment.
This idea is frequently misapplied to ED, which leads to misunderstandings and hinders effective treatment. The involvement of the mind in erections is more extensive, even though some men will have ED as a symptom of underlying mental health disorders like stress.
What the mind believes and how it interprets the world around it helps with erections. Erections will be challenging, if not impossible, to achieve without the right stimulus and desire. The mind must process information in a way that tells the body that an erection is required for sexual interaction, even when external stimulation is present. In the absence of this, ED may occur; not because the mind is interfering with a naturally occurring process, but rather because an essential element of erections (i.e. engaging the mind) is absent.
WHAT CAUSES MENTAL IMPOTENCE?
Although physical factors account for the majority of erectile dysfunction reasons, psychological or emotional problems are also frequently to blame. Erectile dysfunction (ED) or psychological impotence is the term used to describe ED that is caused by a psychological issue.
Erectile dysfunction in males can have a variety of psychological causes, just like with physical ED. Instead, numerous problems can all be the root of or contribute to psychological ED, including:
Anxiety and stress
Despite the fact that stress and anxiety are two distinct conditions, they are nonetheless closely tied to the problem of erectile dysfunction.
Erectile dysfunction frequently has underlying causes that include stress. However, tension can eventually lead to anxiety, which in turn increases stress. This vicious cycle is detrimental for both your mental health and sex life.
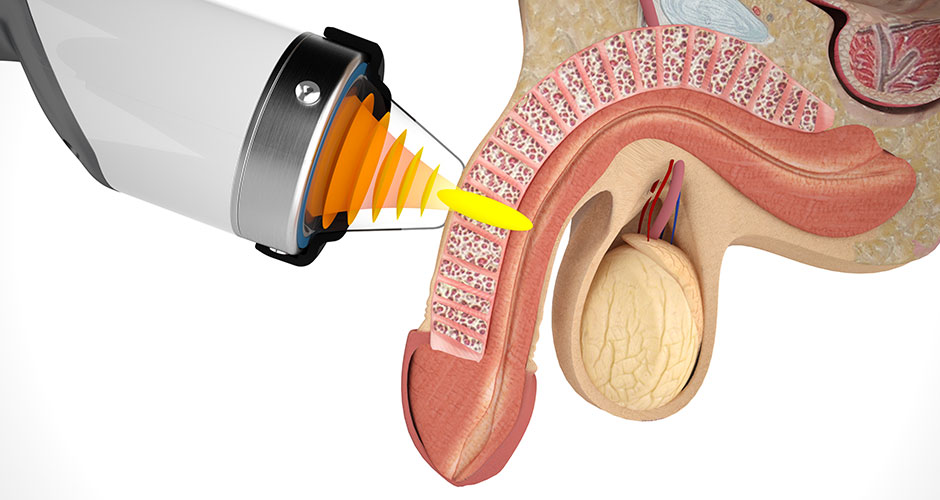
But it’s simple to see that stress and anxiety are much more tightly tied than you might think if you look at the physical side of things. Many guys are unaware that there are actually three different forms of erections.
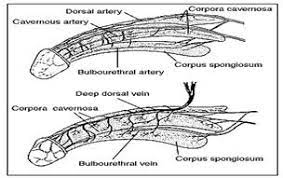
While a psychogenic erection is brought on by a particular visual or mental image, a reflexive erection is brought on by physical stimulus. An erection that takes place while you’re sleeping is known as a nocturnal erection.
Each of these three involves a different set of physiological processes, such as those involving hormones, muscles, blood vessels, the neurological system, and emotions. ED may be brought on by or contributed to by the compromise of any of these systems.
Relationship difficulties
A healthy relationship takes work to develop and keep up. To genuinely know and trust someone, it takes time. It’s possible that problems in your romantic relationship could affect how you and your partner interact sexually.
Another possibility is that your erectile dysfunction is causing issues in your relationship. This is just one example of how the cycle of ED can negatively impact many different areas of your life. The first step in addressing this specific psychological ED cause is communication, but it’s also one of the trickiest.
Participating in counselling may assist you in better understanding each other’s needs and strengthening your relationship if you and your partner have trouble communicating.
Depression
If you haven’t personally dealt with depression, you could imagine it to be similar to melancholy. Clinically, it goes far further than that.
Depression has a similar effect to an anchor, dragging you down mentally and physically and interfering with practically every part of your life. The following are some of the most typical signs of depression:
- constant sadness and emptiness
- feelings of worry, pessimism, or despair about your lot in life
- decreased passion for your hobbies and interests
- feelings of guilt or worthlessness
- slowed speech or movement
- A change in your body weight or appetite
- Oversleeping or have difficulties falling asleep
- inability to concentrate, retain details, or decide
- aches, pains, and stomach problems without a known cause
- Suicidal ideas and actions
As you can expect, these symptoms can make it challenging to enjoy much of anything, much less sex. In middle-aged males, a 1998 study in the journal Psychosomatic Medicine clearly shown a connection between sadness and impotence.
The researchers came to the conclusion that there was an association between depressed symptoms and erectile dysfunction that existed and was unrelated to demographics or ageing using data from the Massachusetts Male Aging Study.
Performance phobia
In many instances, performance anxiety turns into a self-fulfilling prophecy where you worry that you won’t be able to please your spouse. Your anxiety may carry over into the bedroom and contribute to erectile dysfunction.
Negative self-talk, such as fears about being able to get an erection, win over your partner, or refrain from ejaculating too soon, can sometimes be the cause of performance anxiety.
If you’ve had trouble getting an erection in the past, those instances can still be fresh in your memory and interfere with your ability to unwind in bed.
Guilt and low confidence
Many erectile dysfunctional males feel bad about being unable to appease their partner. Guilt can often contribute to the continued cycle of ED if the problem continues to worsen, so it becomes more serious than just a small problem.
Shame and guilt are prevalent emotions that are frequently connected to mental health problems, such as severe depression. In actuality, guilt feelings are a typical sign of depression.
Psychological ED may also be influenced by low self-esteem. Your likelihood of having problems with your sexual performance may increase if you are insecure about it or worry that your partner won’t find you attractive enough.
Use of Pornography
While viewing pornography isn’t necessarily wrong or harmful, it can have a detrimental effect on your sexual function and erectile health.
According to research, regularly watching and masturbating to pornography may lead you to have inflated expectations of your sexual experiences and partners. It’s called porn-induced erectile dysfunction when this makes it harder for you to maintain a hard on.
Conclusion:
Many ED sufferers are uncomfortable with the idea that their thinking is a contributing factor in, if not the main cause of, their inability to have an erection. It may be harder to understand and accept psychogenic ED because it frequently happens even in the absence of any current mental health issues or discomfort.
These guys could be hasty to rule out the idea of psychogenic ED and end up ignoring a crucial aspect of normal erections. However, seeking assistance becomes simpler and ED therapies might ultimately result in greater results when men who experience ED can acknowledge that their minds are constantly engaged throughout erections.
REFERENCES:
- https://www.smsna.org/patients/blog/the-role-of-the-mind-in-erections-and-erectile-dysfunction
- https://www.sharecare.com/health/erectile-dysfunction-causes/brain-play-role-having-erection
- https://austinurologyinstitute.com/blog/psychosocial-impotence-ed-causes/
- https://www.forhims.com/blog/psychological-causes-of-ed
- https://www.healthline.com/health/erectile-dysfunction/psychological