Lets explore the ‘immunity’ secret to living to 100
The number of persons who reach their 100th birthday or older has increased along with the average lifespan of humans.
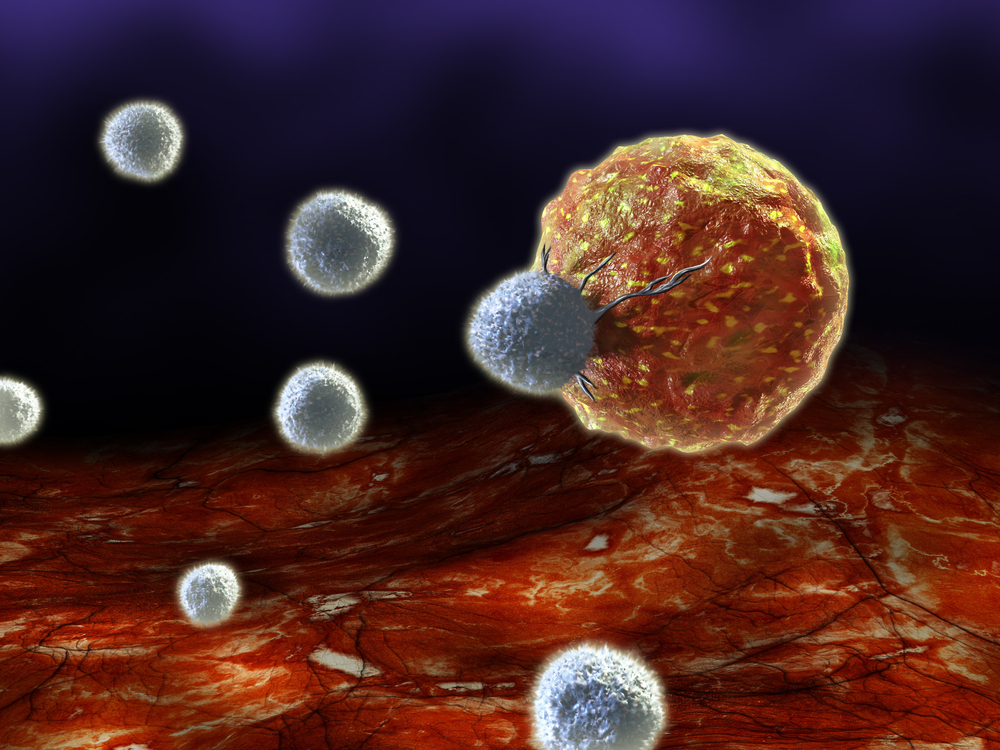
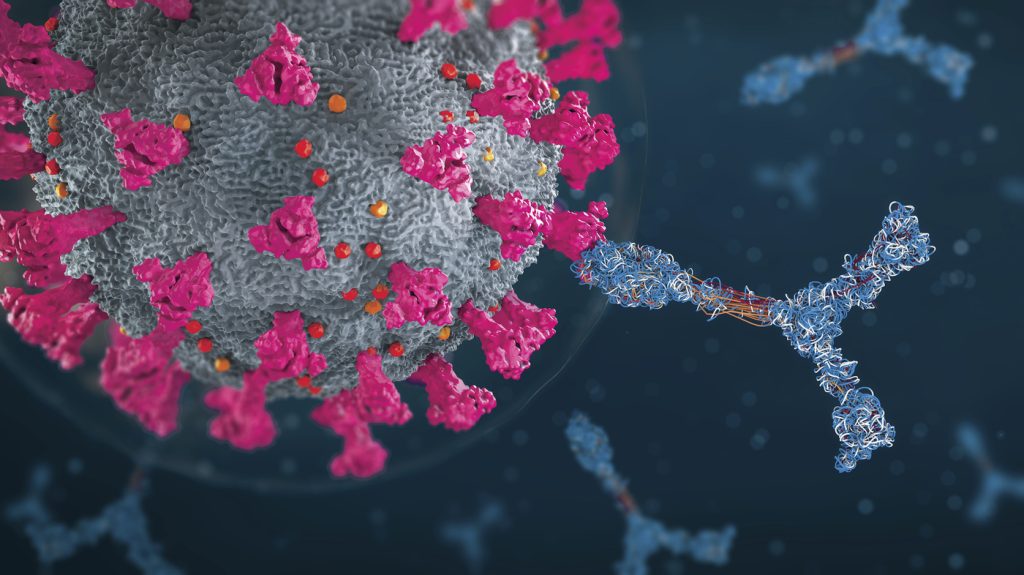
Researchers have discovered that centenarians have a distinct immune cell composition and activity, providing them an immune system that prolongs their lives. These discoveries, according to scientists, may be exploited to create treatments for healthy ageing.
Since 1900, the average human life expectancy has more than doubled. The average lifespan across the globe has increased from 31 years in 1900 to 73.2 years in 2023, and is predicted to reach 77.1 years in 2050.
The proportion of individuals who live to be at least 100 years old is also rising. Researchers predict that by 2050, there will be 3.7 million centenarians, who are known as centenarians, with an estimated 450,000 centenarians worldwide in 2015.
Globally, the number of individuals living to be 100 years or older was predicted to more than quintuple between 2005 and 2030, according to earlier data from the early 2000s. What makes some people able to live beyond their 100s while others cannot is one thing that is still unknown.
This question is being addressed by a recent study that was conducted under the direction of scientists from Tufts Medical Center and Boston University Sachool of Medicine and discovered that centenarians have a distinct immune cell composition and activity that allows them to have a highly functional immune system and live longer.
These results, according to scientists, may be utilised to create treatments that promote healthy ageing. In the most recent issue of Lancet eBioMedicine, the study was published.
Immune system as we age
All bodily systems, including the immune system, undergo changes as we become older.
There are two basic theories on how the immune system changes as we age, according to Dr. Scott Kaiser, a geriatrician and the director of Geriatric Cognitive Health for the Pacific Neuroscience Institute in Santa Monica, California.
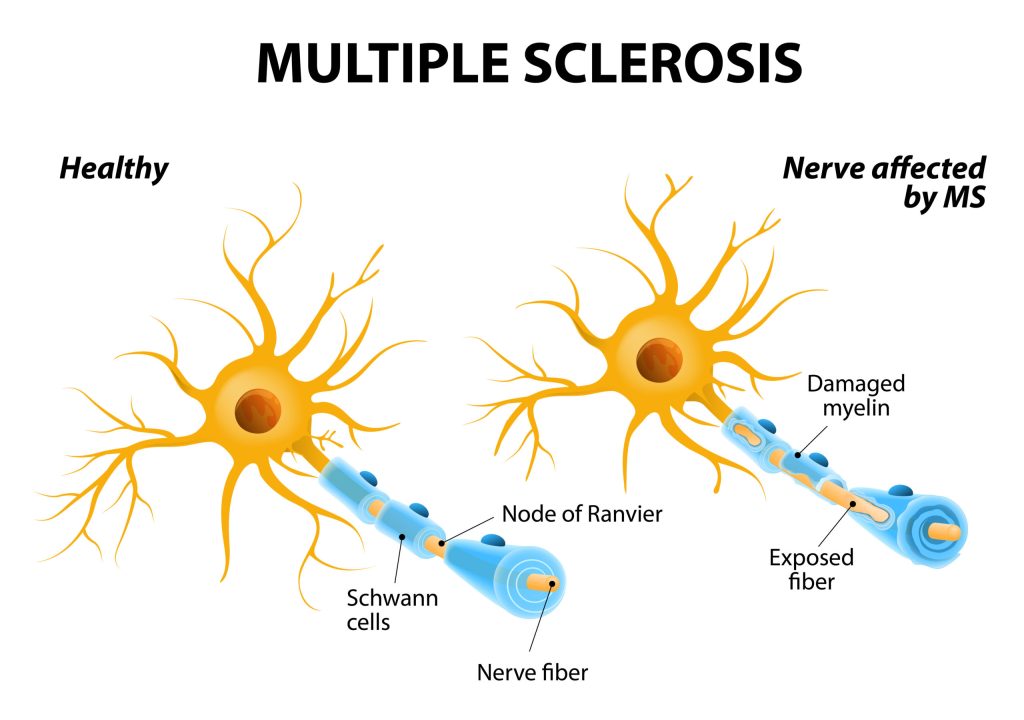
The first is immunosenescence, which he defined as an age-related immunological malfunctioning process. Hence, ageing can cause a decline in immune function due to changes in the makeup and operation of our immune systems. And that’s strongly tied to how susceptible people are to infections, autoimmune conditions, and even different kinds of cancer, he added.
“And then there’s the problem of inflammaging, which is a term that’s been used to characterise age-related increases in inflammation as a result of high levels of pro-inflammatory markers in the blood and other bodily tissues. For example, neurological disorders like Alzheimer’s disease are strongly associated with that risk factor, according to Dr. Kaiser.
There is a lot to consider regarding immune function over time, he continued, and how our immune systems alter with age may either increase our vulnerability or provide protection for us.
A look at a “exceptional” immunity
For this work, blood samples from seven centenarians enrolled in the New England Centenarian Project were used to perform single-cell sequencing on an immune cell subset known as peripheral blood mononuclear cells (PBMCs).
“We examined immune cells that pass through the immune system throughout the human lifespan using single-cell data and novel computational techniques. We examined the existence of particular immune cell types in younger ages and extreme old age and discovered cell type-specific alterations in ageing and extreme old age, according to Dr. Karagiannis.
We also used the same cell types to investigate how gene expression varies with age in order to identify distinct gene expression patterns of extreme longevity that fluctuate with age but are also specific to the very elderly.
Species-specific cell types in centenarians
After investigation, the researchers validated findings from earlier studies on ageing that pointed to distinct compositional and transcriptional alterations for each cell type that are only observed in centenarians and suggest a healthy immune response.
Also, they discovered that both genes with age-related alterations and genes expressed exclusively in centenarians showed cell type signatures unique to remarkable longevity in centenarians.
“Given that centenarians are an ageing population, we weren’t as shocked to uncover genes that change with age in them. What was unexpected were the varied ageing patterns we discovered, including aging-specific genes whose expression levels changed with advancing age but not in extreme longevity across distinct cell populations, according to Dr. Karagiannis
“Our findings can serve as a platform for further research into the causes of extreme old age, which may result in the development of therapies for healthy ageing. To better understand the protective factors of extreme longevity that contribute to the positive health outcomes seen in these people, we would like to examine longitudinal changes in immune cells of centenarians and younger aged persons.
Innovative treatments for disorders associated with ageing
After reading this study, Dr. Kaiser stated that he thought it was interesting because it examined individuals who had aged remarkably well—individuals who had essentially resisted aging—and then examined what was happening in them to see if there was anything we could learn from them.
The possible lessons from this, he said, “are in what makes us more resilient.”
“Looking at these people who had extreme longevity, living into their 100s and even beyond, and determining what is the nature, what is the characteristic of their immune system so that we could better understand what may be going on, and then determining how that could be translated into potential therapies for other people, so that more people can enjoy that”, said Doctor Kaiser
We also discussed this study with Kathleen Cameron, senior director of the Institute for Healthy Aging at the National Council on Aging.
In order to help individuals live longer, she said it’s critical to comprehend the immunological changes related to ageing. And many individuals desire to live longer if it means maintaining their health.
“Treatments that extend life may be developed if we can identify what causes this immunological resilience in those who live to be over 100. Nevertheless, it would also be helpful if there were certain healthy habits that contributed to this resilience, Cameron continued.
She did, however, note that this is all very preliminary data and that further research should be done to help medical professionals comprehend this immunological resilience.
REFERENCES:
- https://www.medicalnewstoday.com/articles/scientists-may-have-found-the-immunity-secret-to-living-to-100
- https://news.yahoo.com/want-live-100-dna-may-184853806.html
- https://baptisthealth.net/baptist-health-news/roundup-april-7-2023
- https://www.unilad.com/news/humans-living-over-100-scientists-study-598021-20230405
For Immune health medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_328