Is Alzheimer’s Disease Detectable by Finger Prick Test?
The ability to diagnose and monitor Alzheimer’s disease remotely may be possible with finger prick tests, according to research.
In contrast to primary care physicians, who only have about 55% accuracy, a different study indicated that blood tests have over 85% accuracy in diagnosing Alzheimer’s disease.
The accuracy and accessibility of diagnosing and managing Alzheimer’s disease may potentially be improved by blood tests.

The number of Americans who have Alzheimer’s disease is currently at 6 million. This number is expected to rise to about 13 million by the year 2050.
Even though there is presently no cure for Alzheimer’s, research have shown that early detection and treatment are essential for postponing the disease’s onset.
Magnetic resonance imaging (MRI), cognitive testing, and physical examinations are currently used as diagnostic techniques. However, access to them is limited because it calls for going to a clinic with knowledgeable staff and involved sample delivery and storage processes.
These tests’ degree of accuracy vary as well. According to a research, almost 25% of people who received a lifetime clinical diagnosis of likely Alzheimer’s had no signs of the disease when they were autopsied.
Furthermore, according to research, up to 50% of dementia sufferers never receive a formal diagnosis while they are still living.
The capacity to detect Alzheimer’s disease earlier and administer treatments that may slow disease development could be aided by increasing the reliability and accessibility of Alzheimer’s testing.
A method for analysing finger prick tests for Alzheimer’s that may be performed at home without a doctor’s supervision was recently developed by researchers.
In contrast to conventional physical examinations, which only accurately diagnose patients with Alzheimer’s disease about 55% of the time, blood tests can detect the disease with a rate of over 85% accuracy.
Alzheimer’s blood tests you can do at home
77 patients from a Barcelona, Spain, memory clinic were involved in the study. All participants gave blood samples from their veins and finger pricks, as well as taking cognitive tests.
For overnight delivery to the University of Gothenburg in Sweden, blood samples were either spotted and dried on “dry blood spot” (DBS) cards or preserved using an anticoagulant called ethylenediamine tetraacetic acid (EDTA).
DBS cards are simpler to carry than EDTA blood samples because they just need to be protected from humidity and moisture. Additionally, centrifugation—the mechanical separation of fluids based on their density—must be performed on EDTA samples before they can be studied, but not on DBS samples.
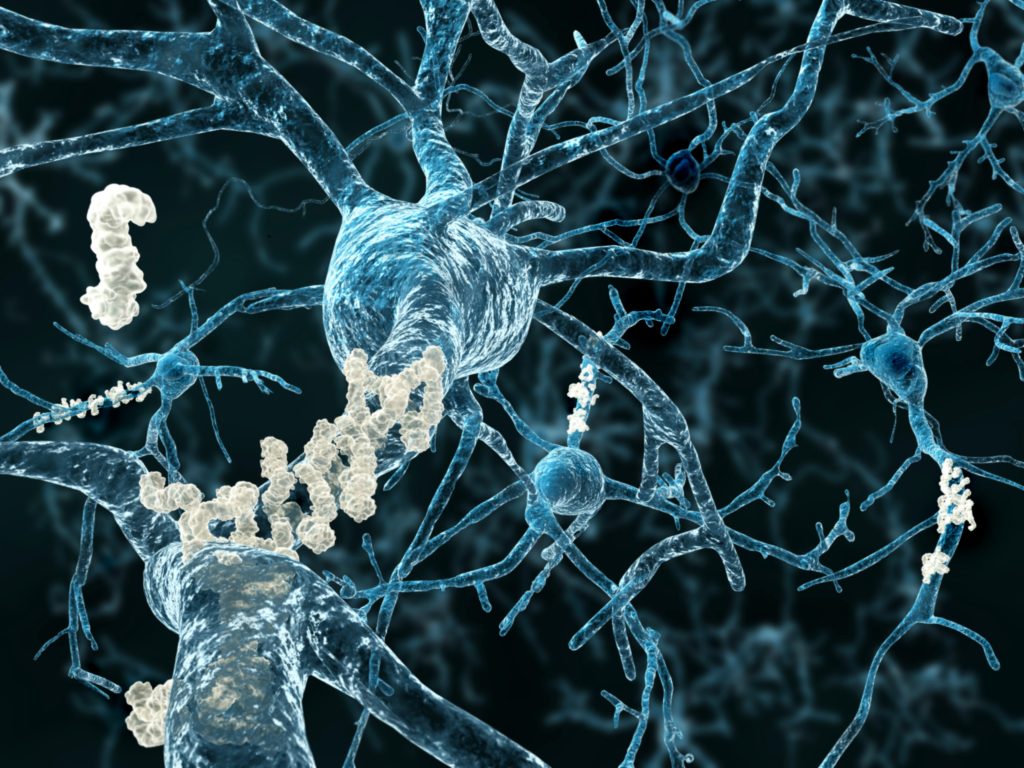
The blood samples were then examined in Sweden for indicators of Alzheimer’s disease, such as phosphorylated tau, glial fibrillary acidic protein (GFAP), and neurofilament light (NfL).
They noticed that all of the blood samples contained indicators for Alzheimer’s disease. As a result, they claimed, Alzheimer’s biomarkers may be measured with finger prick collection, and DBS might facilitate routine monitoring of patients with possible neurological problems.
How precise are Alzheimer’s blood tests?
Dr. Sebastian Palqvist, Ph.D., associate professor at Lund University in Sweden, and colleagues compared the effectiveness of blood-based biomarkers for detecting Alzheimer’s disease with examinations from primary care physicians in a second study that will also be presented at the Alzheimer’s Association International Conference.
They had 307 patients, ranging in age from middle-aged to old, with a mean age of 76. Cognitive evaluations and a CT or MRI scan were part of primary care examinations. Additionally, participants donated a sample of venous blood, which was examined to evaluate the levels of beta-amyloid and phosphorylated tau.
Blood tests accurately detected Alzheimer’s more than 85% of the time, whereas primary care doctors only correctly identified alterations associated with Alzheimer’s 55% of the time.
According to a news release from Dr. Palmqvist, primary care physicians may find it challenging to diagnose Alzheimer’s due to a lack of precise diagnostic equipment.
This too frequently results in misdiagnosis and ineffective therapy. Alzheimer’s blood tests have enormous promise for increasing diagnostic precision and providing patients with the best care possible. In the near future, as new medications that slow the disease in its early stages become more widely accessible, these tests might become even more crucial.
A faster, less expensive method of diagnosis
“We see these new tools improving our ability to recognise the earliest changes of Alzheimer’s and ultimately speeding our ability to prevent or delay the onset of memory decline,” said Dr. Jeffrey Burns, neurologist and co-director of the University of Kansas Medical Center’s Alzheimer’s Disease Research Centre, who was not involved in the study.
“The general public will soon have access to these instruments. We anticipate the FDA approving blood tests for Alzheimer’s within the next one to two years”. Dr. Jeffrey Burns stated, “We are entering a new and exciting era of Alzheimer’s disease with novel diagnostic and treatment options that will significantly alter how we practise.“
Psychiatrist and director of the Pacific Brain Health Centre at the Pacific Neuroscience Institute in Santa Monica, California, Dr. David Merrill, Ph.D., who was not involved in the study, said that there is currently a shortage of specialists who can perform the extensive testing required to diagnose Alzheimer’s.
“Lumbar puncture tests and radioactive brain scans are riskier, more expensive, and require specialised medical care. Even today’s blood tests require specialist processing and handling to prevent results from being tainted,” he said.
“If this method is validated, it could increase the number of patients screened for Alzheimer’s and may help catch the disease early, when interventions can have a greater impact,” said Dr. Jennifer Bramen, Ph.D., a senior research scientist at the Pacific Neuroscience Institute in Santa Monica, California, who was also not involved in the study.
“A simple finger prick of blood put onto a card that can be shipped directly from a patient’s home at room temperature simplifies the process of getting tested for Alzheimer’s,” explained Dr. David Merrill.
Why only a blood test may not be sufficient?
Dr. Bramen pointed out that the findings were limited by the fact that it was a tiny pilot study and that the research procedures and conclusions had not yet undergone peer review.
Detecting amyloid is not the same as diagnosing Alzheimer’s, Dr. Burns continued. It will be crucial to discover the optimal ways to use these technologies in clinical practise, he added.
A neuropsychologist at Baptist Health Marcus Neuroscience Institute named Dr. Raphael Wald, Psy.D., who was not engaged in the study, was also consulted by experts. Although the test may be helpful in corroboration of an Alzheimer’s diagnosis, he pointed out that it does not reveal the severity of an individual’s impairment.
“Some persons can manage their daily lives quite well despite having Alzheimer’s disease as determined by other testing. Others are severely damaged and show no indications of Alzheimer’s,” he said.
Dr. Merrill added that while blood testing might be more accurate than just gathering medical histories, physicians must also think about the care that would follow.
Will confirmatory testing be easily accessible? Who will pay for the test’s repeatability and how often can or should it be performed? Will blood spot testing be recognised as a starting point for therapies, or will additional testing be necessary? How will newly diagnosed patients be supported? Alzheimer’s disease diagnosis can be a heartbreaking event. Before making this test available to the entire public, there are still many details to be resolved,” he said.
REFERENCES:
- https://www.medicalnewstoday.com/articles/a-finger-prick-test-may-help-detect-alzheimers-disease-earlier
- https://www.healthline.com/health-news/can-finger-prick-test-detect-alzheimers-disease-what-to-know
- https://aaic.alz.org/releases_2023/finger-prick-blood-test-alzheimers-disease.asp
For Alzheimer’s disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=31