Issues in an individual’s life dealing with thalassemia
What is thalassemia?
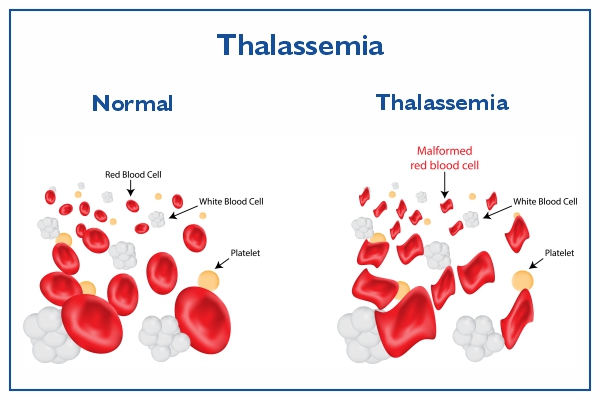
A blood illness called thalassemia causes the body to produce an abnormal kind of haemoglobin. The protein component in red blood cells that carries oxygen is called haemoglobin.
Anemia is brought on by the disorder’s excessive red blood cell oxidation. Your body doesn’t produce enough normal, healthy red blood cells, which is a condition known as anaemia.
Since thalassemia is hereditary, at least one of your parents must have the condition. It results from either a genetic mutation or the loss of specific important gene segments.
A less serious variation of the condition is called thalassemia minor. There are primarily two more severe kinds of thalassemia. At least one of the alpha globin genes has a mutation or other aberration in alpha thalassemia. The beta globin genes are impacted by beta thalassemia.
Different subtypes of these thalassemias exist. The severity of your symptoms and your prognosis will depend on the specific kind you have.
Types of thalassemia
Both the severity of the ailment and the portion of the haemoglobin damaged can be used to classify thalassemia. An individual’s particular kind of thalassemia is typically caused by genetic factors.
Alpha and Beta
Hemoglobin is made up of two beta-globin and four alpha-globin protein chains. Alpha and beta thalassemia are the two primary kinds.
Both parts of the haemoglobin can be impacted by thalassemia, which is sometimes referred to as that part. The term “alpha thalassemia” designates an abnormality of the hemoglobin’s alpha globin chain.
Severity
The degree of the condition is denoted by the phrases “trait,” “minor,” “intermedia,” and “major.” For instance, whereas serious thalassemia may result in severe symptoms necessitating substantial blood transfusions, having the underlying genetic feature for the condition may not cause any symptoms.
Defined terms for identification
The haemoglobin does not create enough alpha protein in people with alpha thalassemia.
Four genes, two on each of the 16 chromosomes, are required for the production of alpha-globin protein chains. Each father gives two to each child. Alpha thalassemia will develop from the absence of one or more of these genes.
The number of mutated genes determines how severe thalassemia is.
- The individual with one mutant gene shows no symptoms. A carrier is a healthy person who has a child exhibiting thalassemia signs. The name for this variety is alpha thalassemia minimum.
- Two genes were altered: He or she has a slight anaemia. It is referred to as minor alpha thalassemia.
- Three genes were altered: Hemoglobin H illness, a form of chronic anaemia, affects the person. Throughout their lifecycle, they will require frequent blood transfusions.
- Four genes were changed: The most severe type of alpha thalassemia is called major. It is understood to induce hydrops fetalis, a dangerous disorder in which fluid builds up in various regions of a fetus’s body.
Four defective genes make it impossible for a foetus to create healthy haemoglobin, making survival even with blood transfusions difficult.
In southern China, Southeast Asia, India, the Middle East, and Africa, alpha thalassemia is a more prevalent form of thalassemia.
A beta thalassemia
For a person to produce beta-globin chains, two globin genes are required, one from each parent. Beta thalassemia will develop if one or both genes are mutated.
How many genes are altered determines the severity.
- An altered gene: It’s known as beta thalassemia mild.
- Two genes were altered: Moderate or severe symptoms are both possible. This is referred to as major thalassemia. It was formerly known as Colley’s anaemia.
People with a Mediterranean background have a higher prevalence of beta thalassemia. In West Asia and North Africa, the prevalence is higher.
Symptoms of thalassemia
Depending on the type of thalassemia, there are different thalassemia symptoms. Symptoms typically start to show in newborns with beta thalassemia and some forms of alpha thalassemia about 6 months of age. This is due to foetal haemoglobin, a unique kind of haemoglobin seen in newborns.
After six months, “normal” haemoglobin begins to replace foetal haemoglobin, and symptoms may start to show. These consist of:
- pale skin and jaundice
- sluggishness and exhaustion
- a chest ache
- breathing difficulty
- quick heartbeat
- sluggish growth
- nausea and lightheadedness
- higher propensity to contract infection
As the body strives to manufacture more bone marrow, skeletal deformations may occur. The iron from blood transfusions may build up. The spleen, heart, and liver can all suffer from too much iron.
Gallstones and an enlarged spleen are more common in people with haemoglobin H, an alpha thalassemia-related blood type. Thalassemia problems that are left untreated have the potential to cause organ failure.
Causes of thalassemia
When one of the genes responsible for producing haemoglobin is faulty or mutated, thalassemia develops. Your parents pass on this genetic aberration to you.
You could develop a condition known as thalassemia minor if only one of your parents is a thalassemia carrier. If it does, you’ll most likely not show any symptoms, but you’ll still be a carrier. Mild symptoms might sometimes appear in patients with thalassemia minor.
You have a higher probability of acquiring a more severe form of the disease if both of your parents are thalassemia carriers.
People from Asia, the Middle East, Africa, and Mediterranean nations like Greece and Turkey are those who have thalassemia the most frequently.
Diagnosis of thalassemia
Your doctor will probably request a sample of your blood to diagnose thalassemia. This sample will be sent to a lab for testing on anaemia and abnormal haemoglobin. Additionally, a lab technician will examine the blood under a microscope to check for abnormally shaped red blood cells.
Thalassemia is indicated by red blood cells with abnormal shapes. The haemoglobin electrophoresis test may also be carried out by the lab technician. By separating the various components in the red blood cells, this test can determine which kind is abnormal.
A physical examination might also assist your doctor in making a diagnosis of thalassemia, depending on the kind and severity of the condition. For instance, your doctor would suspect haemoglobin H illness if you have a substantially enlarged spleen.
Treatment options for thalassemia
The kind and severity of the underlying disease will determine the course of treatment for thalassemia. The optimal course of treatment for your unique situation will be recommended to you by your doctor.
Several of the therapies consist of:
- transfusions of blood
- transplant of bone marrow
- vitamins and medications
- potential spleen or gallbladder removal surgery
Your doctor might advise against taking iron-containing vitamins or supplements. This is particularly true if you require blood transfusions because those who do so build excess iron that the body finds difficult to eliminate. The accumulation of iron in tissues has the potential to be deadly.
Chelation therapy might also be required if you’re undergoing blood transfusions. Typically, a chemical that binds with iron and other heavy metals is injected into the body in order to do this. This aids in getting rid of superfluous iron from your body.
REFERENCES:
- https://www.healthline.com/health/thalassemia
- https://www.medicalnewstoday.com/articles/263489
- https://www.mayoclinic.org/diseases-conditions/thalassemia/symptoms-causes/syc-20354995
- https://my.clevelandclinic.org/health/diseases/14508-thalassemias
- https://www.webmd.com/a-to-z-guides/what-is-thalassemia
For more details, kindly visit below.