Ultrasonic sound helps chemo drugs might treat brain cancer
Because chemotherapy medications cannot cross the blood-brain barrier, brain cancer can be challenging to treat. According to researchers, an ultrasound device has the potential to momentarily remove that barrier and allow chemotherapy medications to get through.
According to experts, this technique could revolutionize the way brain cancer is treated. The most lethal type of brain cancer, glioblastoma, may now be treatable according to recent studies.
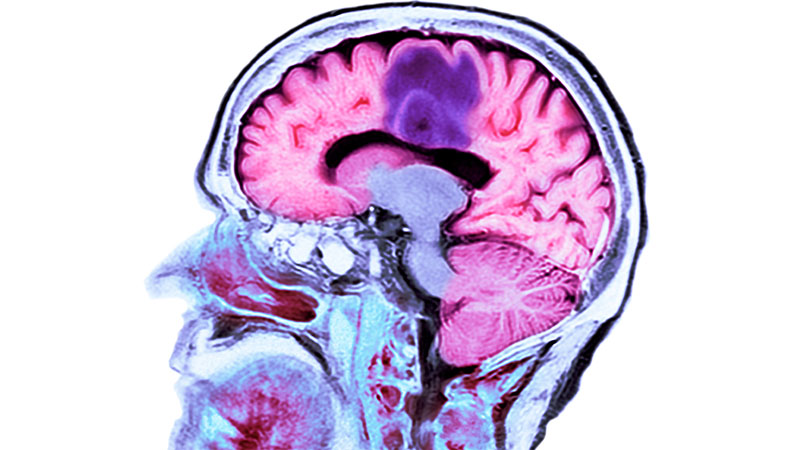
Treatment for brain tumors is very challenging. The blood-brain barrier, which regulates what can travel from the bloodstream to the brain, is a contributing factor in that the majority of chemotherapy medications are inhibited by this barrier.
The issue was overcome by Northwestern Medicine doctors who implanted an ultrasonic device in the brain to momentarily break down the blood-brain barrier, enabling chemotherapy medications to be injected intravenously into the brain.
“Finding that a new technology can safely and effectively open the blood-brain barrier to deliver chemotherapy is potentially a game-changing step forward in brain cancer research and treatment,” Dr. Jason Salsamendi, the lead interventional radiologist at the City of Hope Orange County Lennar Foundation Cancer Centre in California, told us.
Throughout a 4-month period, the 4-minute procedure which is performed on awake patients was repeated once every few weeks for a total of six sessions.
According to the study, which was written up in the journal Lancet Oncology, the surgery caused the concentration of chemotherapy medications in the brain to virtually multiply by four to six.
New brain cancer treatments importance
Dr. Adam Sonabend, a neurosurgeon at the Feinberg School of Medicine at Northwestern University in Illinois, is the study’s primary investigator and neurosurgeon. He also serves as an associate professor of neurological surgery. “While we have concentrated on brain cancer, this provides an opportunity to explore novel drug-based therapies for the millions of patients who are affected by a variety of brain diseases,” the authors write.
Dr Albert Kim, director of the brain tumour centre at Washington University in St. Louis’ Siteman Cancer Centre, who was not involved in this trial, told us that systemic distribution via IV is typical and simple to carry out.
Although the blood-brain barrier had previously been opened with ultrasound, Kim stated that “the implantable device allows for repeated openings, which could enable the delivery of multiple cycles of systemic drugs.”
The trial included paclitaxel and carboplatin, two powerful chemotherapy medications that are typically ineffective in the treatment of glioblastoma.
Temozolomide, the major chemotherapeutic agent now being used to treat glioblastoma, can cross the blood-brain barrier, however it is somewhat ineffective.
Injecting paclitaxel directly into the brain has been shown in prior studies to be beneficial, but it also carries the risk of meningitis and irritated brain tissue.
The five-year survival rate for glioblastoma is now at around 10%, and patients have not benefited from recent developments in cancer treatment, such as targeted medicines and immunotherapy, according to Salsamendi. An option to administeradminister medication directly into the brain each time a dose is needed is the ability to distribute chemotherapy across the blood-brain barrier.
Blood-brain barrier being opened
The blood-brain barrier quickly closed after being forced open, often within 30 to 60 minutes, according to the study’s researchers.
Salsamendi noticed that there is a greater possibility of dangerous substances entering the brain if the blood-brain barrier is breached for a longer period. In terms of treatment planning and risk minimization, it would be important to know how long the barrier may be open with as much accuracy as feasible.
The French biotech company Carthera created the ultrasound device, which breaks down the blood-brain barrier via a stream of tiny bubbles.
One hour later, the blood-brain barrier recloses.
The researchers found that the blood-brain barrier may be temporarily opened in people using ultrasound and microbubble technology and that most of its integrity returns an hour later.
The brain is permeable to medications circulating in the bloodstream for a critical period of time following sonification, according to Sonabend, who is also a member of Northwestern University’s Robert H. Lurie Comprehensive Cancer Centre.
The blood-brain barrier is fully restored 24 hours after brain sonication, according to prior human investigations. However, the field previously made the assumption that the blood-brain barrier is open during the first six to eight hours. According to the Northwestern study, this window may be smaller.
Another first is that the blood-brain barrier is opened in a brain volume that is nine times greater than the initial device (a modest single-ultrasound emitter implant) when a revolutionary skull-implantable grid of nine ultrasound emitters created by the French biotech company Carthera is used. This is crucial because for this method to be effective, a sizable area of the brain close to the cavity that remains after the excision of glioblastoma tumours must be covered.
REFERENCES:
- https://www.medicalnewstoday.com/articles/chemotherapy-drug-reaches-brain-in-humans-for-first-time
- https://news.northwestern.edu/stories/2023/05/chemotherapy-drug-reaches-brain-in-humans-for-first-time/
- https://www.livescience.com/health/brain-cancer/new-ultrasound-device-helps-powerful-chemo-reach-deadly-brain-cancers-human-trial-shows
- https://www.upi.com/Health_News/2023/05/03/Ultrasound-procedure-allows-chemo-to-reach-the-brain/2801683122296/
For Cancer disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=10