Bottom line on bronchitis and its various treatment.
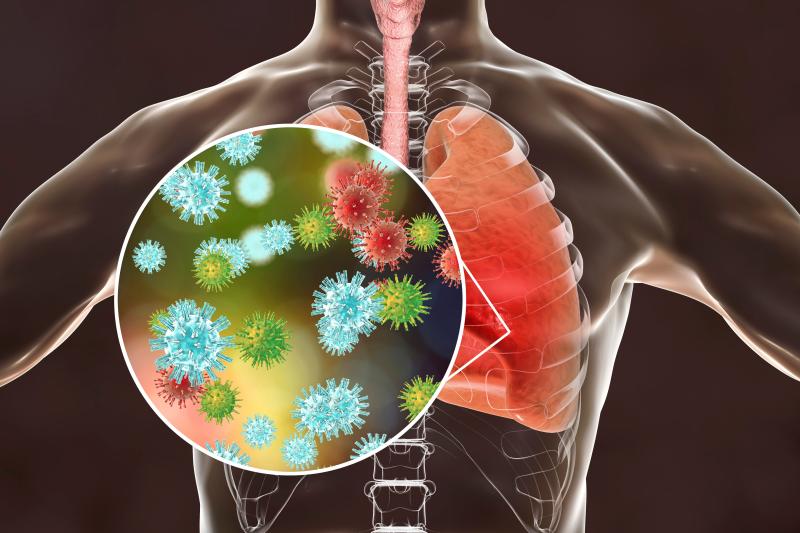
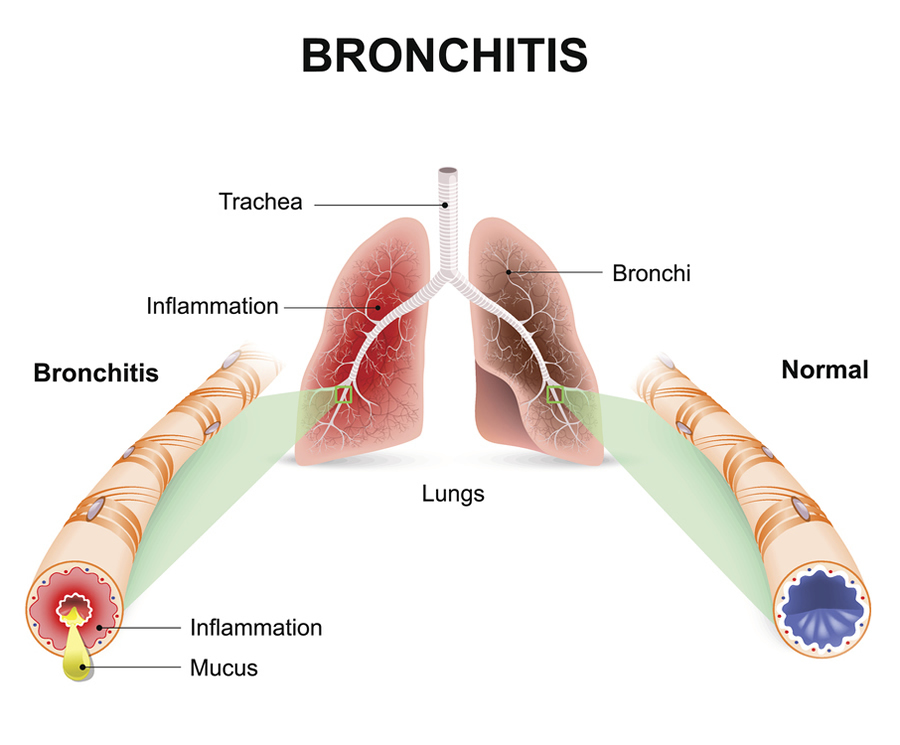
In people with bronchitis, the airways that connect the mouth, nose, and lungs experience swelling and irritation. A cough, wheezing, and trouble breathing are bronchitis symptoms. Additionally, individuals may struggle to clean their airways of thick mucus or phlegm.
You can have acute or chronic bronchitis. Acute bronchitis typically goes away on its own, but chronic bronchitis persists and never fully heals. Bronchitis can be avoided by not smoking or by quitting altogether.
Symptoms and Types of Bronchitis
You can have acute or chronic bronchitis. If the condition is acute, it only occurs once before a person recovers. Even if it may occasionally get better and worse, if it is chronic, a person must always deal with it.
Both acute and chronic bronchitis have the following symptoms:
- a chronic cough that occasionally produces mucous
- wheezing
- chills and a low fever
- a sensation of chest constriction
- an upset stomach
- bodily pains
- breathlessness
- headaches
- clogged sinuses and nose
If the bronchial tubes take a long time to heal completely, a person with bronchitis may have a cough that lasts for several weeks or even a few months. Chronic bronchitis symptoms can recur frequently. This occurs frequently for many people during the winter.
Nevertheless, bronchitis is not the only illness that results in a cough. A persistent cough could indicate asthma, pneumonia, or a number of other illnesses. For a diagnosis, anyone with a recurrent cough should visit a doctor.
Acute bronchitis
A certain amount of time is required to treat acute bronchitis. It frequently has a similar pattern to a viral infection, such the flu or a cold, and it might be caused by the same virus.
The individual could:
- a cough, whether or not it is mucous
- chest pain or discomfort
- fever
- bodily aches and a little headache
- breathing difficulty
In most cases, symptoms disappear after a few days or weeks.
Chronic bronchitis
Although chronic bronchitis is a continuing condition, it exhibits symptoms similar to acute bronchitis. According to one definition, someone has chronic bronchitis if they cough productively every day for two or more years in a succession and for at least three months out of the year.
It is classified as a kind of chronic obstructive pulmonary disease (COPD) in which the bronchial tubes create a lot of mucus, according to the National Library of Medicine. Either it stays put or it leaves but keeps returning.
According to the Centers for Disease Control and Prevention (CDC), someone who develops emphysema combined with chronic bronchitis will be given the diagnosis of COPD. A dangerous and maybe fatal condition, this one.
Who does bronchitis affect?
Everyone can get bronchitis, however several factors put you at greater risk:
- smoke or spend time with smokers.
- have COPD, asthma, or another respiratory disorder.
- own GERD (chronic acid reflux).
- possess an autoimmune condition or another inflammatory disease.
- are nearby air contaminants (like smoke or chemicals).
Diagnosis of bronchitis
A stethoscope will be used by the doctor during the physical examination to listen for any strange sounds coming from the lungs.
They might also inquire of someone about:
- their signs, particularly the cough
- their medical background
- any recent cold or flu symptoms
- or not they smoke
- exposure to air pollution, dust, fumes, or secondhand smoke
The physician could also:
- to check for bacteria or viruses in the lab, obtain a sputum sample.
- assess the person’s blood oxygen levels.
- suggest a pulmonary lung function test, a chest X-ray, or blood testing
Treatment of bronchitis
A bronchitis patient may be advised by a doctor to:
- rest
- ingest liquids
- ingest over-the-counter (OTC) drugs, like ibuprofen
Taking over-the-counter medication will help you get rid of a cough and any related pain. Acute bronchitis will eventually go away, frequently untreated.
For a period, the signs of chronic bronchitis may go away or get better. But if there is exposure to smoking or other triggers, they will return or get worse again.
Options that could be useful include:
- Cough medicine: While medication can offer comfort, especially at night, coughing is still helpful in clearing mucus from the bronchial tubes.
- Online retailers sell cough medications.
- Honey consumption: Two spoonfuls of honey may help with cough symptoms.
- Using a humidifier: It can help to reduce wheezing, increase airflow, and release mucus.
- Bronchodilators: These help to remove mucus by widening the bronchial passages.
- Mucolytics: These facilitate sputum production by thinning or loosening mucus in the airways.
- Steroid and anti-inflammatory medications: These can aid in reducing inflammation, which can lead to tissue damage.
- Oxygen therapy: In serious conditions, a person may require additional oxygen to help them breathe easier.
Behavioural cures
The following are additional bronchitis treatment options:
- removing, say, a lung irritant by not smoking
- strengthening the chest muscles through exercise will aid with breathing
- pulmonary rehabilitation improves breathing technique
Breathing exercises like pursed-lip breathing can assist slow breathing down and improve its efficiency.
Antibiotics
A doctor may advise antibiotics if a bacterial infection causes acute bronchitis. In some circumstances, taking antibiotics may also help avoid a secondary illness. However, a person with a virus should not use these medications.
Most medical professionals won’t recommend antibiotics until they know that bacteria are to blame for the patient’s ailment. Antibiotic resistance is one of the causes of this, as excessive antibiotic use makes it more difficult to treat an infection over the long term.
How to prevent pneumonia?
Even though you may not be able to prevent bronchitis, there are certain things you can do to reduce your risk. These consist of:
- avoiding irritants such as smoke
- obtaining a seasonal influenza vaccine
- Using handwashing to stop the transmission of germs
- obtaining lots of sleep
- eating a balanced diet
REFERENCES:
- https://www.healthline.com/health/bronchitis-symptoms
- https://www.medicalnewstoday.com/articles/8888
- https://www.mayoclinic.org/diseases-conditions/bronchitis/symptoms-causes/syc-20355566
- https://my.clevelandclinic.org/health/diseases/3993-bronchitis
- https://www.webmd.com/lung/understanding-bronchitis-basics
For more details, kindly visit mbelow.