Cancer: physical activity a day could lower your risk.
In a recent study, the impact of vigorous intermittent lifestyle physical activity (VILPA) on the risk of developing cancer was examined.
Using information from wrist-worn accelerometers, researchers followed 22,398 non-exercisers’ health records for cancer for nearly 7 years while also tracking their daily intense activity.

When compared to not participating in VIPLA, 4.5 minutes of VILPA per day, divided into 1-minute bursts, was linked to a 32% lower chance of developing cancer.
Power walking, lugging groceries, and climbing stairs are just a few examples of the many possibilities that exist in daily life for strenuous physical activity.
The importance of physical activity to overall health and wellbeing cannot be overstated. According to research, regular exercise can reduce the risk of developing chronic diseases like cancer, diabetes, and cardiovascular disease.
In fact, the World Health Organisation (WHO) reports that those who are not adequately active have a death risk that is 20–30% higher than those who are.
Even though the benefits of physical activity are obvious, only about 1 in 3 women and 1 in 4 men globally adhere to the guidelines for 75 minutes of strenuous exercise or at least 150 minutes of moderate exercise per week.
Good news has arrived from a recent study for those who dislike or are unable to engage in structured, intense exercise.
Just 4.5 minutes per day of vigorous-intensity physical exercise undertaken in 1-minute bursts was related with an up to 32% decreased risk of cancer, according to wrist-worn accelerometer data taken from 22,398 non-exercising people collected from the UK Biobank.
VILPA: What is it?
Short bursts of physical activity that are a regular component of our lifestyle (daily living) are referred to as vigorous intermittent lifestyle physical activity (VILPA) by Dr. Stamatakis and his colleagues.
VILPA examples include, but are not restricted to:
- climbing hills
- ascending stairs
- power walking, also known as maximising walking pace for a short distance (like 100–200 metres) to reach intense intensity, involves carrying children or groceries for 50–100 metres.
- intense housework.
- VILPA differs from conventional intense physical activity in that it is intermittent and transient, lasting up to two minutes at a time, as opposed to continuous and planned.
Effects of VILPA and cancer risk
The study was a prospective cohort study of adults, aged 40 to 69, who provided the UK Biobank with their data.
The research team led by Dr. Stamatakis only included participants from the accelerometer-wearing group who reported not exercising in their free time and taking one or fewer leisurely walks per week in their analysis of the association between VILPA and cancer incidence.
The study removed participants who provided incomplete information, had a history of cancer, or improperly wore the activity monitor.
22,398 participants made up the study population, and their average age was 62. 54.8% of these were female, and 96% of them were white.
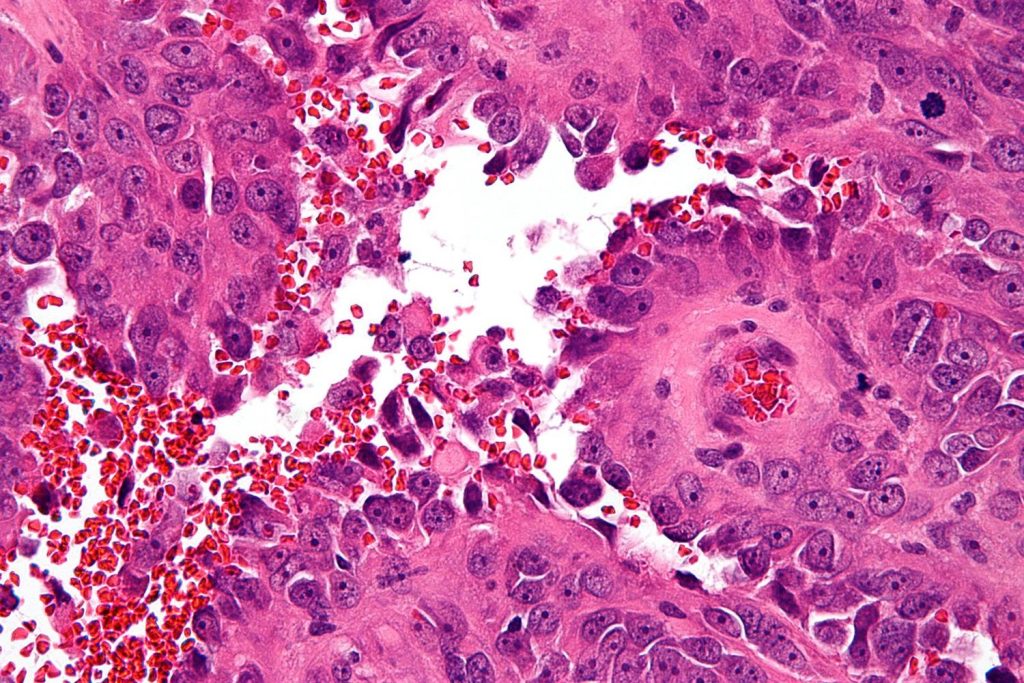
The researchers found 2,356 new cancer occurrences throughout a mean follow-up period of 6.7 years, including cancer registration, hospitalisation for cancer, or death from any malignancy.
The researchers utilised a machine-learning method known as “random forest” to categorise accelerometer-recorded physical activity based on intensity — vigorous, moderate, and light.
VILPA reduces cancer risk by just a few minutes every day.
The majority of VILPA incidents took place in spurts of up to one or two minutes. People participated in VILPA for a maximum of 16 minutes, or about 4.5 minutes per day on average.
According to statistical assessments, the association between VILPA and cancer risk is almost linear, meaning that a person’s risk of developing cancer decreases as they engage in more VILPA.
People who engaged in VILPA for an average of 4.5 minutes per day, in short bursts of up to 1 or 2 minutes, had a 20% lower chance of developing cancer than those who did not engage in any VILPA (6.2% of study participants).
Previous studies have demonstrated a link between insufficient physical activity and several cancer forms. These consist of:
- liver
- lung
- kidney
- gastric cardia (a type of stomach cancer)
- endometrial
- Leukaemia myeloid
- myeloma
- colorectal
- neck and head
- bladder
- mammary cancer
- esophageal adenocarcinoma (esophageal cancer)
This study demonstrates that those who engaged in 4.5 minutes of VILPA daily have a 31% lower risk of developing certain physical activity-related malignancies.
The least amount of VILPA necessary to significantly lower the chance of developing cancer was also determined by the researchers. They discovered that 3.4 minutes of VILPA per day can reduce the risk of cancer overall by 17% and 3.6 minutes of VILPA per day can reduce the risk of cancer linked to physical activity by 18%.
More study is required to determine how VILPA affects cancer.
A relatively small quantity of strenuous lifestyle activity can have such a large link with decreased cancer risk, according to the “high-quality study,” according to Dr. David Raichlen, professor of biological sciences and anthropology at the University of Southern California.
According to him, “the authors used a novel machine learning-based method to identify behaviours and this study moves the field forward, allowing us to better understand the benefits of this form of physical activity on [the] risk of developing cancer.”
Because of the study’s methodology, Dr. Raichlen advised that causality could not be established; however, “this work certainly suggests that future intervention studies using VILPA are warranted.”
According to Prof. Markus Gruber, chair of Training and Movement Science and director of the University Konstanz’s Human Performance Research Centre, the study supports the long-held belief in exercise science that “intensity matters.”
Prof. Gruber made the same observation as Dr. Raichlen, namely that although the study’s data, methods, and analysis are sound, the study is cross-sectional and can only report relationships between VILPA and cancer incidence.
When challenged about the connection between VILPA and cancer incidence, Prof. Gruber responded that there are a number of plausible “explanations for the results that need to be tested.”
He claims that VILPA may either directly lower the risk of cancer, boost physical fitness, or show superior physical fitness, which is linked to a lower risk of cancer. Additionally, VILPA may reduce the effects of aging-related fitness decreases and reduce cancer risk by doing so.
Overall, according to Prof. Gruber, VILPA is a promising substitute for duration-based advice on physical activity, “especially for people who don’t like to exercise.”
REFERENCES:
- https://www.medicalnewstoday.com/articles/5-minutes-physical-activity-lowers-cancer-risk
- https://www.wsj.com/articles/even-four-minutes-of-exercise-a-day-could-cut-your-cancer-risk-8768087f
- https://www.prevention.com/health/health-conditions/a44690519/4-5-minutes-vilpa-workout-daily-lowers-cancer-risk-study/
For Cancer disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=10