What are the ways to treat and diagnose Gastritis?
What is Gastritis?
Gastritis is a disorder that causes the mucosa lining of the stomach to become inflamed. This inflammation results in stomach pain, dyspepsia, bloating, and nausea. It can trigger other issues. Gastritis can develop gradually (chronic) or suddenly (acute) (chronic). Reducing stomach acid and modifying your diet can help with gastritis symptoms.
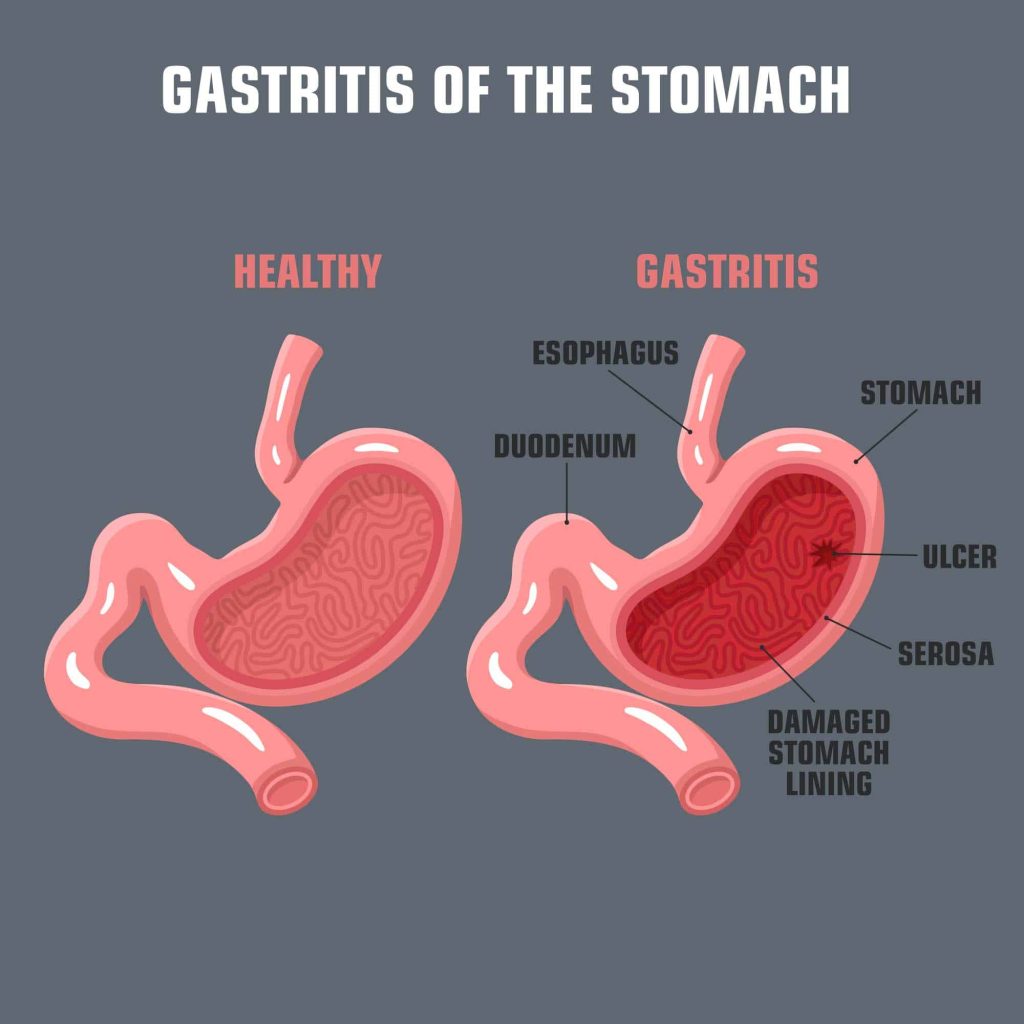
The mucosa is the protective mucus lining that lines your stomach. Your stomach’s lining shields it from the powerful stomach acid that aids in food digestion. The protecting mucosa gets inflamed and leads to gastritis when something weakens or harms it. The most frequent bacterial cause of gastritis is a kind of bacterium known as Helicobacter pylori.
About 8 out of every 1,000 people get acute (sudden) gastritis. Long-term, chronic gastritis is less frequent. Approximately two out of every 10,000 people are impacted.
Types of Gastritis
There are two main categories of gastritis:
Erosive (reactive): Erosive gastritis results in both stomach lining erosion and inflammation. Reactive gastritis is another name for this illness. Alcohol, smoking, NSAIDs, corticosteroids, viral or bacterial infections, stress from diseases or injuries, and corticosteroids are some of the causes.
Non-erosive: Stomach lining inflammation that does not cause erosion or compromise the lining.
What Causes Gastritis?
Inflammation brought on by heavy alcohol use, frequent vomiting, stress, or the use of specific medications like aspirin or other anti-inflammatory therapies can result in gastropathy. Additionally, it might result from any of the following:
- Abuse of alcohol: Prolonged drinking can irritate and damage the stomach lining.
- Autoimmune disease: In certain people, the stomach lining’s healthy cells are attacked by the immune system.
- Bacterial infection: Peptic ulcer illness and chronic gastritis are mostly brought on by the H. pylori bacterium (stomach ulcers). Inflammation is brought on by the bacteria’s destruction of the stomach’s barrier lining.
- Reflux of bile: Your liver produces bile to aid in the digestion of fatty foods. Reflux is a reflowing action. When bile bypasses the small intestine and instead rushes back into the stomach, this condition is known as bile reflux.
- Medication: Regularly taking corticosteroids or nonsteroidal anti-inflammatory medications (NSAIDs) to treat chronic pain can irritate the stomach lining.
- Stress on the body: A sudden, serious sickness or injury might cause gastritis. Gastritis frequently occurs even following trauma to the body that does not affect the stomach. Brain injuries and severe burns are two common causes.
Symptoms of gastritis
There are many cases of gastritis without symptoms. When symptoms do occur, many people mistake them for indigestion. Additional indications of gastritis include:
- tarry, dark stool
- Bloating.
- vomiting and nauseous.
- greater satiety during or after a meal.
- decrease in appetite.
- abdominal ulcers
- shedding pounds without intending to.
- discomfort or soreness in the upper abdomen (belly).
- throwing up blood.
How is gastritis diagnosed?
Your doctor will examine you physically and inquire about your medical history and symptoms. Your doctor might also recommend one or more of the following tests:
- Breath test: You ingest a capsule or liquid containing the radioactive substance urea during an H. pylori breath test. Then you exhale into a bag that resembles a balloon. Urea is converted into carbon dioxide by H. pylori bacteria. The breath test will reveal a rise in carbon dioxide if you have the bacteria.
- Blood test: Checking for antibodies that combat the H. pylori bacteria through a blood test.
- Stool test: H. pylori bacteria are detected in your stool during this test of your faeces (poop).
- Upper endoscopy: Your doctor examines your stomach using an endoscope, a lengthy, thin tube with a camera attached to it. The oesophagus, which joins your mouth to your stomach, is where the doctor puts the scope. Using an upper endoscopy, your doctor can look at the stomach lining. Additionally, a tissue sample (biopsy) from the lining of your stomach may be taken in order to check for infection.
- Upper GI examination: For an upper GI examination, you ingest barium, a chalky material. Your stomach lining is coated by the fluids, giving the X-ray technician more precise images.
How is gastritis treated?
Depending on the reason, there are many treatments for gastritis. While some medicines treat symptoms of dyspepsia, others kill bacteria. Your healthcare professional might advise:
Antibiotics: The bacterial infection may be treated with antibiotics. For a few weeks, you might need to take many different kinds of antibiotics.
Antacids: Calcium carbonate drugs that act as antacids lessen exposure to stomach acid. They could aid in reducing inflammation. Heartburn can also be treated with antacids like Tums and Rolaids.
Histamine (H2) blockers: Drugs like ranitidine (Zantac), cimetidine (Tagamet), and other analogues reduce the formation of stomach acid.
Proton pump inhibitors: These drugs lessen the amount of acid your stomach generates. Examples include omeprazole (Prilosec) and esomeprazole (Nexium). Proton pump inhibitors also treat gastroesophageal reflux disease and stomach ulcers.
REFERENCES:
- https://www.mayoclinic.org/diseases-conditions/gastritis/symptoms-causes/syc-20355807
- https://www.webmd.com/digestive-disorders/digestive-diseases-gastritis
- https://my.clevelandclinic.org/health/diseases/10349-gastritis
- https://medlineplus.gov/ency/article/001150.htm
For more details, kindly visit below.