Important note on gum diseases and its treatment.
A non-destructive form of periodontal disease is gingivitis. This condition is sometimes referred to as gum disease. Early gum disease known as gingivitis often has minimal symptoms.
The main forms of gingivitis are two. Dental plaque buildup irritates the gums, causing swelling, discolouration, and pain. This condition is known as plaque-induced gingivitis.
In contrast, bacterial, viral, or fungal infections can cause non-plaque-induced gingival lesions. This kind of gingivitis can also be brought on by infections, allergies, and reactions to foreign objects like dentures.
If either kind of gingivitis is not appropriately treated, it might develop into periodontitis. A more serious condition, periodontitis, can cause additional problems, like tooth loss.
Types of gum infections
In most cases, tooth plaque buildup is what causes gingivitis. Inadequate dental hygiene is only one of several potential contributing variables, which also include:
- a few drugs, including oral or injectable birth control, cyclosporine, calcium channel blockers, and phenytoin (these medications can cause gingivitis or make it worse because they can lead to an overgrowth of gum tissue and make plaque hard to remove)
- severe vitamin C deficiency (this is rare in the United States)
- hormonal changes, such as those that occur during pregnancy and menopause
- leukaemia
- nickel, a hefty metal that is used in various jewellery
- exposure to bismuth, a substance present in several cosmetics
Some gum infections that result in gingivitis are unrelated to plaque accumulation. These consist of:
- some viral or fungal illnesses, like thrush
- a tooth that is impacted, or one that doesn’t fully emerge (if this happens, the flap of gum over the tooth can trap debris and cause gingivitis)
What causes gingivitis?
In contrast to what we see, your gums actually join your teeth at a place below the gum line. This creates a little void known as a sulcus. An accumulation of food and plaque in this area might result in gingivitis or a gum infection.
Bacterial thin film is known as plaque. It continuously develops on your teeth’s surface. Tartar develops as plaque hardens over time. Plaque that penetrates below the gum line might cause gum infection.
Gingivitis can cause the gums to split from the teeth if it is not treated. This may lead to:
- harm to the teeth’s supporting bone and soft tissue
- the tooth to become fragile and loose
- the tooth’s eventual loss if the illness spreads
Risk factors for gingivitis
Risk factors for gingivitis and periodontitis include the following:
- Using tobacco to smoke or chew
- diabetes
- several drugs, including:
- oral conceiving pills
- steroids
- anticonvulsants
- blockers of calcium channels
- chemotherapy
- Uneven teeth
- an inadequate fit for dental appliances
- faulty fillings
- pregnancy
- genetic influences
- weakened immunity, such as that caused by HIV
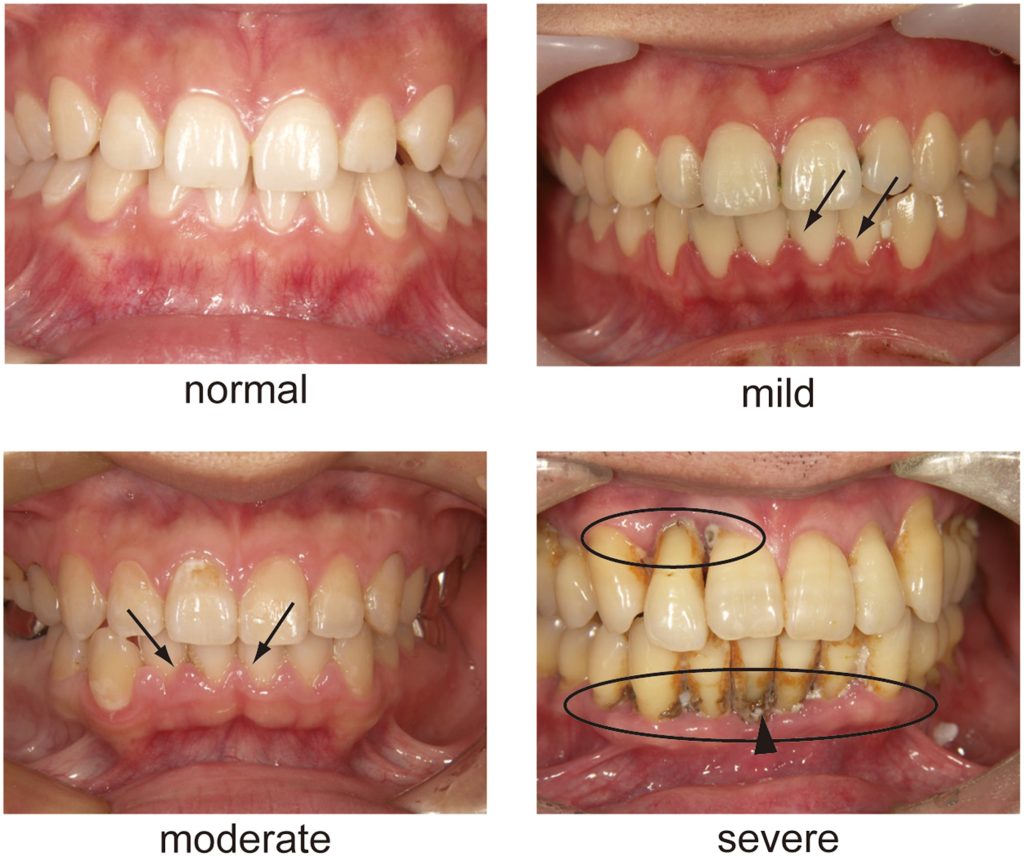
Symptoms of gingivitis and periodontitis
The majority of people are unaware they have gum disease. Gingivitis can exist without showing any symptoms. However, the following signs of gum disease can occur:
- Symptoms of red, painful, or swollen gums
- bleeding gums during tooth brushing or flossing
- gums that are no longer attached to your teeth
- tooth decay
- a modification in the way your teeth bite together (malocclusion)
- pus between the gums and teeth
- difficulty chewing
- vulnerable teeth
- no longer fitting partial dentures
- bad breath that persists even after brushing your teeth
How is Gum disease diagnosed?
Your gums will be prodded with a small ruler during a dental examination.
- By probing, you can examine the area for inflammation.
- Any pockets around your teeth are measured. 1 to 3 millimetres is a normal depth.
- X-rays may also be requested by your dentist to check for bone loss.
Discuss your symptoms and the causes of your gum disease with your dentist. This could be used to identify gingivitis. If gingivitis is present, a periodontist may be consulted. A dentist who focuses on the treatment of gum disorders is known as a periodontist.
How is gingivitis treated?
To treat gingivitis, you must maintain good oral hygiene. Additionally, if you smoke, you should reduce your intake, and if you have diabetes, you should take care of it. Even though giving up smoking can be challenging, a doctor can assist you in creating a strategy that will work for you.
Other therapies comprise:
- dental hygiene routine
- antibacterial drugs
- surgery
- brushing teeth
Numerous methods can be utilised to thoroughly clean your teeth without surgery. To avoid causing gum inflammation, they all eliminate plaque and tartar:
- Scaling. Tartar from both above and below the gum line is removed by teeth scaling.
- Root thinning. By doing so, the root surface’s rough patches are smoothed down and plaque and tartar are removed.
- Lasers. In comparison to scaling and root planing, this procedure may eliminate tartar with less discomfort and blood.
Medications
Gum disease can be treated with a variety of drugs:
- Chlorhexidine-containing antiseptic mouthwash can be used to clean your mouth.
- After root planning, pockets can be filled with timed-release antiseptic antiseptic chips containing chlorhexidine.
- After scaling and planing, antibiotic microspheres produced with minocycline can be placed into pockets.
- Inflammation of the gums that persists can be treated with oral antibiotics.
- An antibiotic called doxycycline helps prevent enzymes from harming teeth.
Surgery
You may require surgery if your gingivitis is severe, especially if it has led to any bone or gum tissue loss. A periodontist can perform several different kinds of gum surgery, including:
- flap surgery During a flap surgery, the gums are pulled back and tartar and plaque are removed from deeper places. The gums are then positioned around the tooth and secured with sutures.
- tissue and bone transplants. When your teeth and jaw are too damaged to repair, grafting may be necessary.
- To conceal the exposed tooth root, gum graft surgery takes tissue from your mouth’s roof. This lessens further bone and gum deterioration.
- Your doctor will begin a bone graft operation similarly to a flap procedure, but they will insert a bone graft to help your body replace any missing jaw bone.
- lengthening of dental crowns. There may be more gum tissue in some gingivitis sufferers. A periodontist can remodel your gum and bone tissue in this situation so that more of your teeth are visible. Additionally, it could be required prior to some dental restoration or cosmetic operations.
REFERENCES:
- https://www.mayoclinic.org/diseases-conditions/periodontitis/symptoms-causes/syc-20354473
- https://www.webmd.com/oral-health/guide/gingivitis-periodontal-disease
- https://my.clevelandclinic.org/health/diseases/21482-gum-periodontal-disease
- https://www.medicalnewstoday.com/articles/241721
- https://www.healthline.com/health/gingivitis
For more details, kindly visit below.