How can loneliness affect bone health in males?
The impact of social isolation on bone loss in mice was examined by researchers. They discovered that social isolation increased bone loss in male mice, but not in female mice.
To determine whether the same occurs in humans, more research is required. Poorer health outcomes, such as an increase in all-cause mortality, cardiovascular issues, and mental health issues, are associated with social isolation.

Psychological stress has also been connected to risk factors in previous studies.reputable source for information on osteoporosis and weak bones.
Social isolation, which is closely related to loneliness, can cause mental suffering. The relationship between social isolation and bone health is still unclear, though.
Researchers recently looked into how social isolation impacts the bone health of male and female mice. They discovered that in male mice, but not in female mice, social isolation was linked to bone loss.
The research was introduced in Chicago at ENDO 2023, the Endocrine Society’s annual meeting. The study’s non-participant assistant professor of geriatrics at McGovern Medical School at UTHealth Houston, Dr. Nahid Rianon, was our source for information on the results.
Lead author of the study and postdoctoral fellow at MaineHealth Institute for Research’s Centre for Molecular Medicine, Dr. Rebecca Mountain, also provided the following information to us.
Future research is required to fully understand the effects on humans, but the findings “may also have clinical implications as we grapple with the long-term health impacts of the rise in social isolation related to the COVID-19 pandemic.”
The bone density was decreased in isolated mice.
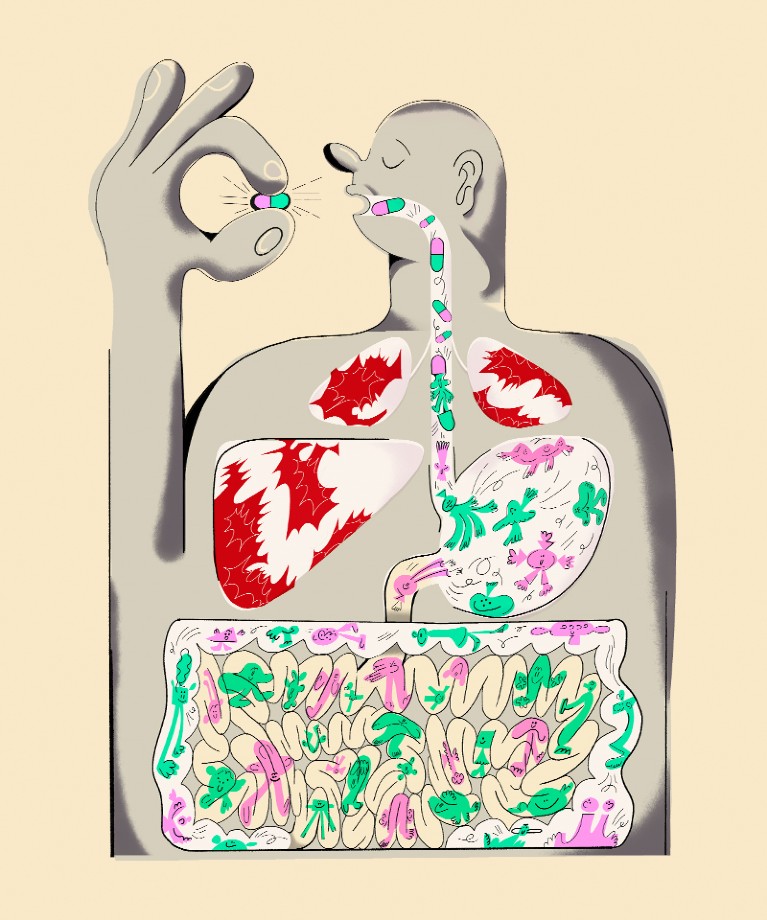
32 male and female mice aged 16 weeks were divided into two groups for this investigation. One mouse per cage was used in one group’s simulation of social isolation. Four mice shared one cage in the other group.
The mice were observed by the researchers in their separate environments for 4 weeks. Finally, the bone mineral density of solitary male mice decreased. Less dense and therefore more likely to break, bones with fewer minerals are less dense.
Additionally, the researchers discovered that in solitary male mice, bone volume fraction and cortical bone thickness decreased by 26% and 9%, respectively. Both measurements point to a decline in bone quality.
Further investigation found that male mice showed impaired bone remodelling, which includes the production of new bone and raises the risk of fracture.
The scientists observed that the bone loss seen in guys who were kept alone was comparable to that shown in earlier studies after orchiectomy (removal of the testicles) and ovariectomy (removal of the ovaries).
In contrast, there was no bone loss after social isolation in the present study’s female mice.
However, despite the fact that their bone mass was unaltered, the researchers discovered that isolated females exhibited higher bone resorption-related gene expression. Increased bone resorption can cause bones to degrade more quickly than they can regenerate, raising the risk of fracture.
Underlying processes
Dr. Mountain pointed out that it is unknown exactly how social isolation may cause bone loss. Her team is investigating many hypotheses, including the function of various stress hormones and the sympathetic nervous system of the body.
We also discussed the mechanisms underlying the effects of social isolation on bone health with Dr. William Buxton, a board-certified neurologist and the director of Neuromuscular and Neurodiagnostic Medicine and Fall Prevention at Pacific Neuroscience Institute at Providence Saint John’s Health Centre in Santa Monica, California, who was not involved in the study.
“My initial reaction to the connection is that performing weight-bearing workouts is one of the finest methods to preserve bone health and fend off osteoporosis. One is less inclined to leave their home if they are isolated, and as a result, they are less likely to be on their feet, he explained.
“Both depression and weight loss can result in frailty, disability, and decreased mobility, which can contribute to bone loss,” continued Dr. Rianon. Future study is required to understand the underlying metabolic alterations that cause bone loss in various medical diseases, as they are all risks for bone loss.
Why is there a sex difference?
Dr. Mountain mentioned that they are currently looking into why social isolation had distinct effects on men and women. She mentioned that oestrogen is known to protect bones, suggesting that it might be involved.
It’s also plausible that male and female mice experience solitude on different time scales or in various ways, she added.
We also discussed the sex disparities with Dr. Douglas Landry Jarvis, an orthopaedic surgeon with Novant Health in Charlotte, North Carolina, who was not involved in the study.
The synthesis of testosterone and hormonal balances may have been disrupted by a lack of social engagement, which would have had a negative impact on bone metabolism. Over a 4-week period, the female hormonal cycle may be less impacted.
Study restrictions
The study’s weaknesses, according to Dr. Mountain, are its small sample size and lack of behavioural information on how isolation influenced mice’s depressive or anxious behaviour.
Dr. Buxton said that the study’s use of caged animals meant that it was not a perfect representation of human behaviour. I don’t know if the authors documented how frequently the animals in the cages were on their feet, but I would anticipate that the community animals would be more mobile.
Dr. Rianon continued by saying that although the study suggested that male and female mice may have different bone-forming processes, it does not specify how these variations arise.
Nevertheless, she added, “It’s pretty normal to not have [such] details in the early stages of any research.”
Research implications for the future
Dr. Buxton added, “I also guess that alcohol plays a role if these results are later demonstrated in humans.”
“We are aware that drinking makes osteoporosis more likely. Alcohol is probably a link between isolation and lower bone mineral density in individuals because isolation is a risk factor for increased alcohol consumption“, the scientist hypothesized.
According to the study, no one should alter their routines, Dr. Jarvis continued. The study’s sole recommendation is that more research be done. The variable of social engagement is too broad. The amount by which the mice’s cortisol levels changed will determine if the study can be generalized to primates and perhaps even humans.
REFERENCES:
- https://www.medicalnewstoday.com/articles/could-loneliness-impact-bone-health-in-males
- https://www.editorji.com/lifestyle-news/health/loneliness-may-be-bad-for-men-s-bones-too-study-1687154981821
- https://www.arnnewscentre.ae/news/lifestyle/lonelinesss-impact-on-mens-bone-health-highlighted-in-new-study/
For Bone disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=63