Quick peek of study in the Deep Vein Thrombosis (DVT).
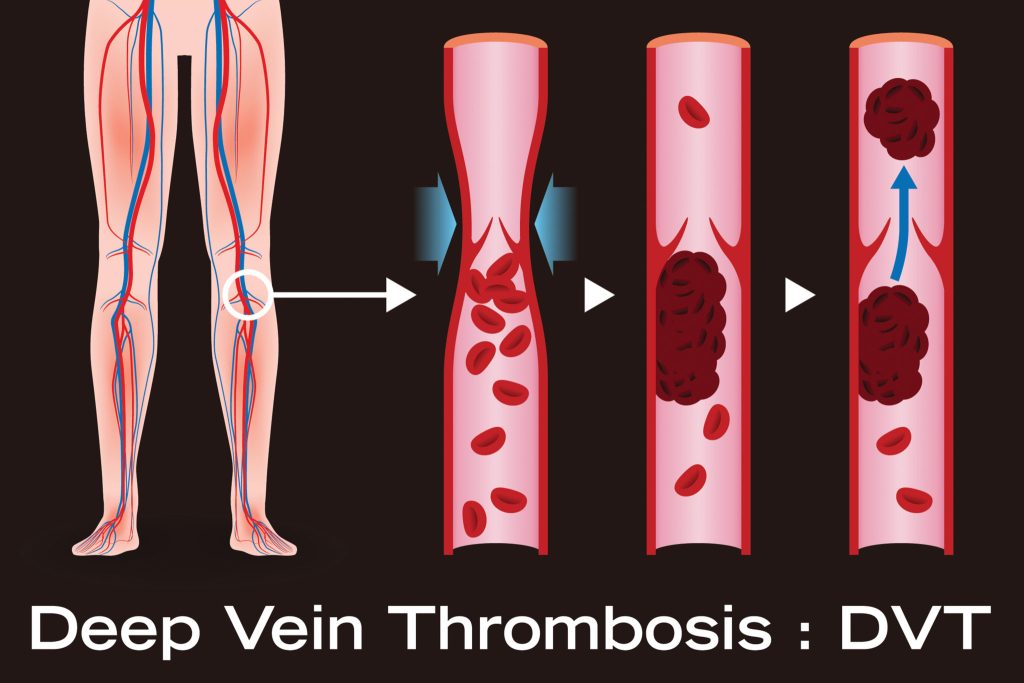
Blood clots commonly form in a deep vein in the leg, which is where deep vein thrombosis occurs. The disorder can also affect pelvic veins in addition to leg veins. The condition known as venous thromboembolism includes the conditions of deep vein thrombosis (DVT) and pulmonary embolism (PE).
A medical emergency is DVT. According to the Centers for Disease Control and Prevention (CDC), 10–30% of persons with DVT in the leg die within a month of their diagnosis due to severe consequences.
What is Deep Vein Thrombosis (DVT)?
Blood clotting known as DVT occurs in deep veins, frequently in the pelvis or leg. Doctors refer to a thrombus or blood clot breaking off as an embolus. A PE can develop if emboli reach the lung.
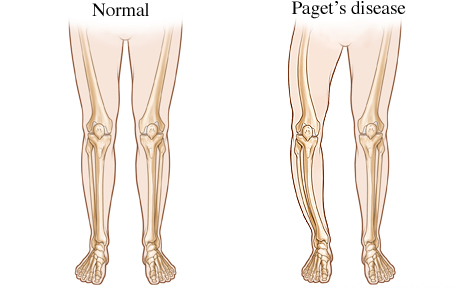
As in the case of those who have Paget-Schotter illness, clots can also form in the arm veins. DVT is the most frequent reason for maternal death in the industrialised world, according to a 2017 analysis.
DVT in children is incredibly uncommon. The most recent statistics, according to a 2016 study, indicate that 0.30 of every 100,000 children under the age of nine and 0.64 of every 100,000 children between the ages of 10 and 19 get DVT.
DVT symptoms
Only about half of DVT patients, according to the Centers for Disease Control and Prevention (CDC), experience symptoms. Typical DVT signs include:
- swelling on one side of your leg, ankle, or foot
- cramping pain, which typically starts in the calf, in the affected leg.
- acute, irrational foot and ankle pain
- a patch of skin that feels warmer than the rest of the body
- depending on skin tone, the skin over the affected area becomes pale, reddish, or bluish in hue.
People who have an arm blood clot or an upper extremity DVT may not exhibit any symptoms. If they do, typical signs include:
- a stiff neck
- shoulders hurt
- the hand or arm swelling
- deeper or bluer tinge to the skin
- from the arm to the forearm moving discomfort
- fragility in the hand
It’s possible for someone to discover they have DVT only after receiving emergency care for a pulmonary embolism (blood clot in the lung).
A DVT clot that has entered the lung from the arm or leg may cause a pulmonary embolism. It is life threatening and necessitates immediate medical attention when an artery in the lung becomes blocked.
Causes and risk factors
A blood clot is the root cause of DVT. The clot prevents blood from flowing through a vein and into your body normally. Various things can cause a DVT or raise the chance of getting one.
They consist of:
- Injury: Blood flow can be restricted or blocked when a blood vessel’s wall is damaged. As a result, a blood clot may develop.
- Surgery: Blood vessels may be harmed during surgery, which may cause a blood clot to form. Following surgery, bed rest with minimal to no activity may potentially raise your chance of developing a blood clot.
- Reduced mobility or inactivity: Blood can accumulate in your legs, especially the lower ones, when you sit regularly, such on a lengthy flight. The blood circulation in your legs may dwindle if you are immobile for a lengthy amount of time. This may lead to the formation of a clot.
- A few drugs: Some medications make it more likely for your blood to clot. These include antidepressants, glucocorticoids, hormone treatment medications, and birth control pills.
- Age: DVT can occur at any age, however it is more common as people get older. DVT only occurs in 1 in 10,000 people under the age of 20, whereas it occurs in 1 in 100 people beyond the age of 80.
- Trauma: A blood clot may form as a result of a wound that weakens your veins, such as a bone fracture.
- Obesity. Being overweight might increase strain on the veins in your pelvis and legs.
- Pregnancy: DVT risk is higher during pregnancy. Actually, compared to non-pregnant people, pregnant people have a 5–10 times higher risk of developing DVT.
- Family history: If you have DVT, you may be more prone to get it.
- Catheter: Inserting a catheter into a vein can make it more likely for a blood clot to form.
- Smoking: This is linked to an increased risk of DVT.
Additionally, a number of other medical disorders can raise the risk of DVT.
These consist of
- inflammation of the colon
- Blood clotting diseases
- high blood pressure and heart failure are cardiac issues
- sepsis
- Cancer
- Tuberculosis, Covid-19, and other viral or bacterial diseases
- asthma
- sleep apnea
- polycystic ovary syndrome (PCOS)
- diabetes
Complications of DVT
Pulmonary embolism is one of the main side effects of DVT. If a blood clot travels to your lungs and clogs a blood vessel, you could have a pulmonary embolism.
Your lungs and other organs could suffer severe harm as a result. Immediately seek medical attention if you experience any pulmonary embolism symptoms. These indicators include:
- dizziness
- sweating
- coughing or taking big breaths causes chest pain that intensifies
- quickly breathing
- spitting blood
- quick heartbeat
Treatments of DVT
Some DVT sufferers may require inpatient treatment. Others might be eligible for outpatient care.
Compression stockings, elevating the affected leg(s) during the day, and taking anticoagulant drugs (blood thinners) are all forms of treatment. In rare instances, intrusive therapies (catheter-based procedures) may be necessary when the DVT is severe.
The main objectives of treatment include:
- Ensure that the clot doesn’t spread or include other veins.
- Avoid having a venous clot fragment escape and travel to your lungs.
- reduce the possibility of a new blood clot.
- Prevent long-term complications from the blood clot (like chronic venous insufficiency).
Prevention of DVT
Many required modifications are included into a healthy lifestyle to stop blood clots from forming. This entails increasing physical activity, giving up smoking, and maintaining a healthy weight. Your risk of developing DVT can also be decreased by:
- control of blood pressure
- quitting smoking
- keeping a healthy weight
In order to reduce your risk of getting clots following surgery, take whatever blood thinners your doctor recommends. When you sit for longer than four hours, your chance of getting DVT increases.
When you’ve been sitting for a while, moving your legs around will also keep your blood circulating. After being confined to bed, getting up and moving around can stop clots from developing. During long travels, get out of the vehicle and take regular breaks to stretch.
REFERENCES:
- https://www.healthline.com/health/deep-venous-thrombosis
- https://www.medicalnewstoday.com/articles/153704
- https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/symptoms-causes/syc-20352557
- https://my.clevelandclinic.org/health/diseases/16911-deep-vein-thrombosis-dvt
- https://www.webmd.com/dvt/what-is-dvt-and-what-causes-it
For more details, kindly visit below.