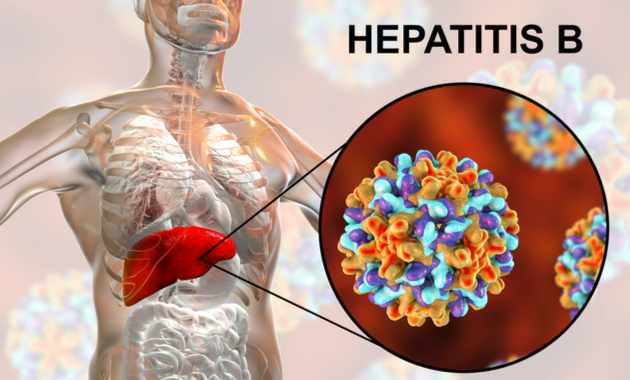
Important causes and symptoms of Hepatitis B.
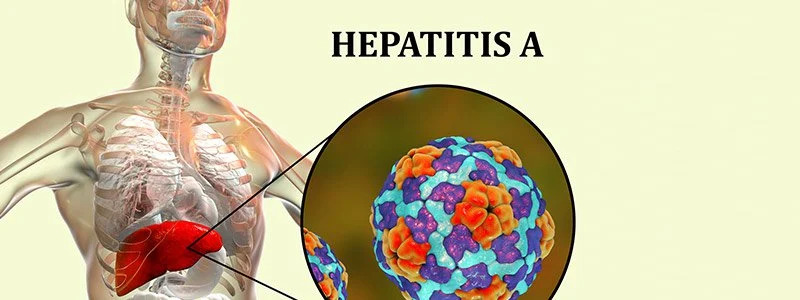
What is hepatitis B?
A liver infection known as hepatitis B is brought on by the hepatitis B virus (HBV). One of the five varieties of viral hepatitis is HBV. Hepatitis A, C, D, and E make up the other four. Each one is a distinct kind of virus. The most likely types to develop chronic or long-lasting are types B and C.
Around 296 million individuals worldwide are thought to be infected with hepatitis B, according to the World Health Organization. In 2019, around 1.5 million new cases of chronic hepatitis B were reported.
Acute or chronic HBV infection are both possible. Adults with acute hepatitis B experience sudden onset of symptoms. Rarely do newborns who receive hepatitis B at birth simply experience acute symptoms. The majority of baby hepatitis B infections progress to chronic disease.
What are the types of hepatitis B?
Hepatitis B infections come in two flavours: acute and chronic.
Acute
When you contract hepatitis B for the first time, an acute infection occurs. Many people can get it out of their bodies and feel better. In fact, roughly 4 out of 5 sick adults fit this description.
Chronic
You have chronic hepatitis B if you are unable to get rid of the virus within six months or longer. (Chronic denotes continual.) The dangerous, sometimes fatal diseases of liver cancer and cirrhosis of the liver are caused by chronic hepatitis B, which also causes inflammation. Treatment can halt the progression of the condition, lower the risk of developing liver cancer, and improve survival rates.
What are the symptoms of hepatitis B?
Acute hepatitis B symptoms can not show up for several months. However, typical signs include:
- fatigue
- dark faeces
- muscle and joint ache
- reduced appetite
- fever
- digestive discomfort
- weakness
- yellowing of the skin and eye whites (jaundice)
An early evaluation is required for any hepatitis B symptoms. Acute hepatitis B symptoms worsen in those over 60. If you believe you may have been exposed to hepatitis B, tell your doctor right once. It’s possible that you can stop an infection.
How common is hepatitis B?
According to the WHO, around 296 million people around the globe live with chronic HBV. Around 1.5 million new infections occur every year.
According to the Centers for Disease Control and Prevention (CDC), chronic hepatitis B affects approximately 1.2 million people in the United States.
But HBV often goes undetected. In fact, the WHO estimates that only about 10.5% of people living with hepatitis B were aware of their condition as of 2019.
Causes and risk factors for hepatitis B
A viral infection called hepatitis B can be spread by blood or other body fluids like vaginal or sperm.
Hepatitis B can be spread, among other things, by:
- having intercourse without using a condom or other barrier techniques with a person who has HBV
- sharing blood-contaminated razors, nail clippers, or toothbrushes
- getting a tattoo or a body piercing with unsterilized equipment
- sharing needles, syringes, or other supplies while injecting narcotics
- from a parent giving birth to a newborn child
Although the virus may be found in the saliva, hepatitis B is not transmitted through:
- kissing
- sneezing
- coughing
- sharing cutlery
HBV infection is more likely to occur in some groups than others. These comprise of:
- medical professionals
- users of injectable medications
- infants conceived by HBV-positive parents
- HBV-positive individuals’ sexual partners
- people with renal disease who are on dialysis
Complications of hepatitis B
Chronic hepatitis B complications include:
- the hepatitis D virus
- hepatic scarring (cirrhosis)
- liver damage
- liver tumour
- death
Only those who have hepatitis B can get hepatitis D. Although hepatitis D is rare in the US, it can also cause chronic liver disease.
REFERENCES:
- https://www.healthline.com/health/hepatitis-b
- https://www.webmd.com/hepatitis/digestive-diseases-hepatitis-b
- https://my.clevelandclinic.org/health/diseases/4246-hepatitis-b
- https://www.who.int/news-room/fact-sheets/detail/hepatitis-b
- https://www.mayoclinic.org/diseases-conditions/hepatitis-b/symptoms-causes/syc-20366802
For more details, kindly visit below.