Is Covid-19 linked to a rising risk of developing diabetes?
The question of whether or not viral infections can raise the chance of getting diabetes has been the subject of research for some time.
The virus that causes COVID-19, SARS-CoV-2, has now prompted scientists to investigate whether diabetes risk can be raised by SARS-CoV-2 infection.
According to recent data, the COVID-19 pandemic may have contributed to a 3-5% rise in the overall disease burden of diabetes in the Canadian population.
In order to prevent further injury to those who have been harmed, this evidence supports requests for greater observation of blood sugar levels in COVID-19 survivors.
The complete impact on the health of the worldwide population has not yet been fully appreciated, although the COVID-19 pandemic has so far caused close to 7 million fatalities, according to the World Health Organisation (WHO).
COVID-19 and diabetes association
This is not the first time that research has drawn attention to a possible connection between diabetes and SARS-CoV-2 infection.
American retrospective cohort research that was published in the BMJ in May 2021 showed that people who become infected have a considerably higher risk of diabetes. A prior article in Nature demonstrated an increased likelihood of metabolic diseases, including diabetes, being diagnosed after an illness.
The ability of SARS-CoV-2 to infect human pancreatic cells—which produce insulin and are harmed and eventually destroyed in diabetics—was proven later that year in a study published in the journal Cell Metabolism. The loss of these cells could potentially be caused by infection, suggesting a potential underlying mechanism to explain the relationship.
Since then, cohort studies have indicated a greater incidence rate of type 2 diabetes, but not type 1 diabetes, after infection. One such study was reported in Diabetologia. Another retrospective cohort study employing Veterans Health Administration data, which was published in Diabetes Care, revealed that males, but not women, saw a rise in the incidence of all diabetes diagnoses following SARS-CoV-2 infection.
Children are more likely to be diagnosed with type 1 diabetes than adults are, according to a cohort study that was published in PLOS One. The risk of type 1 diabetes diagnosis after infection was also found to be higher in American Indian/Alaskan Native, Asian/Pacific Islander, and Black populations.
Diabetes is 22% more likely to develop
Now, a study involving 629,935 persons, with an average age of 32, has found that men who tested positive for SARS-COV-2 between January 1, 2020, and December 31, 2021, had a 22% higher risk of developing diabetes in the eight months after infection than men who hadn’t been exposed.
Based on age, sex, and date of infection, researchers matched pairings of individuals with a confirmed case of COVID-19 and those who hadn’t, using data from the British Columbia COVID-19 Cohort, a database of SARS-CoV-2 infection in British Columbia, Canada.
When the results were stratified by the severity of the disease, researchers discovered that those who had COVID-19 when they were admitted to the hospital had a 2.4-fold increased risk of developing diabetes compared to those who hadn’t been infected, and those who were admitted to intensive care had a 3.29-fold increased risk.
When these cases were taken into account, the data revealed that women were also more likely to acquire diabetes following infection with SARS-CoV-2, albeit this tendency was not significant when only moderate cases were taken into account.
The scientists were unable to differentiate between type 1 and type 2 diabetes using the data they had access to since this link was only discovered for non-insulin-dependent diabetes.
Risk of diabetes with viral infections
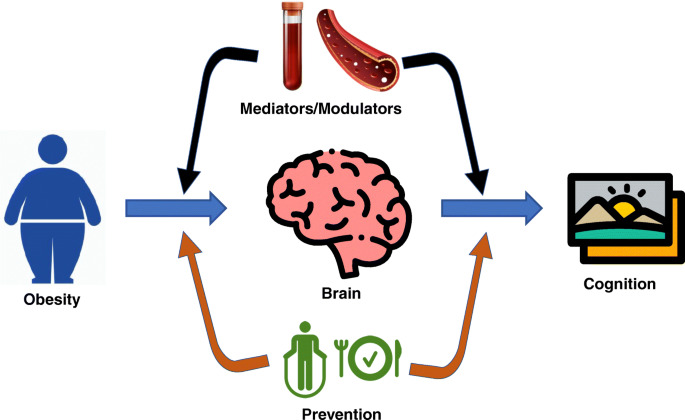
It is unclear precisely how SARS-CoV-2 infection causes these long-term consequences, as it is with other long-term side effects. It is not the first time that a viral infection has been connected to a higher chance of acquiring diabetes, but the mechanisms underlying the association are still unknown.
The effect of Coxsackievirus B infection on the risk of type 1 diabetes has been extensively investigated, along with the effects of mumps, rubella, and cytomegalovirus, according to Dr. Fares Qeadan, associate professor of biostatistics at Loyola University Chicago who was not involved in the study.
Researchers have also looked into the potential roles of inflammation, insulin resistance, and impacts on pancreatic cells in the relationship between hepatitis C virus infection and the risk of type 2 diabetes.
In conclusion, viral infections have been linked to a higher risk of developing both type 1 and type 2 diabetes. The evidence for type 1 diabetes is stronger and includes a wider range of viruses, but the data for type 2 diabetes is more limited and mostly concentrates on particular viral diseases like the hepatitis C virus. Dr. Fares Qeadan stated that more study is required to pinpoint the precise processes by which viral infections influence the onset of diabetes and to create preventative measures.
Diabetes or long COVID, which is it?
As the clinical characterisation of long-COVID is still being developed, experts cautioned that it was a complicated topic to determine whether the onset of diabetes following infection with SARS-CoV-2 might be regarded a symptom of long-COVID.
Dr. Morgan Birabaharan, a physician and virus researcher from the University of California, San Diego’s Division of Infectious Diseases and Global Public Health who was not involved in the study, stated:
The onset of diabetes may fall within the category of protracted COVID, which is used to characterise a variety of symptoms and illnesses that appear after the acute phase of SARS-CoV-2 infection (>30 days).
To classify what side effects of SARS-CoV-2 infection are ‘long COVID’ vs. some other process, he said, “is difficult because we are still trying to understand the pathophysiology of long COVID, whether it be persistent viremia, dysregulated immune response, or some other phenomenon.”
This most recent article backed suggestions for aggressive management of this, saying that the population-level effects of a rise in diabetes cases caused by the COVID-19 pandemic could also be considerable.
In any case, Dr. Qeadan said, “Recognising the potential link between SARS-CoV-2 infection and the onset of diabetes is important for healthcare professionals as it highlights the need for careful monitoring of blood glucose levels and early intervention in people who have had COVID-19.”
“This can help lessen the long-term effects of diabetes on the affected individuals and reduce the overall burden on healthcare systems,” he continued.
After COVID, diabetic symptoms
Increased thirst and hunger, frequent urination, unexplained weight loss, exhaustion, and hazy eyesight are all typical early indicators of diabetes, according to Ricordi.
If you had COVID-19 and any of these symptoms, it would be worthwhile to request a diabetic screening from your doctor, especially if you have risk factors or a family history of the disease.
One should see their primary care physician if any of these symptoms or indicators are present, according to Ricordi.
The conclusion
An increased risk of diabetes has been linked with COVID-19, according to recent research. Diabetes may be another factor contributing to extended COVID, according to the study. Endocrinologists think COVID-19 may harm the pancreas and affect how it releases insulin, though additional research is required to fully understand the association.
REFERENCES:
- https://www.medicalnewstoday.com/articles/covid-19-linked-to-increased-risk-of-developing-diabetes
- https://www.healthline.com/health-news/diabetes-risk-may-increase-40-after-having-covid-19
- https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02656-y
- https://www.nature.com/articles/d41586-022-00912-y
For Diabetes medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=13