Important signs to consider to avoid Colorectal cancer.
The incidence of colorectal cancer, which ranks third among all cancers in the globe, is on the decline in older people and is largely avoidable. However, the prevalence of colorectal cancer among younger people is rising.
Seven risk factors that raise the likelihood of colorectal cancer in younger males have been found in a recent study. Men under 45 who are at increased risk should get screened for colorectal cancer, according to the authors.
Colorectal cancer is the third most prevalent cancer in the world, behind breast and lung cancer. Only lung cancer accounts for more fatalities. It is estimated that each year, more than 150,000 people in the United States alone receive a colorectal cancer diagnosis.
The median age of diagnosis for colorectal cancer is 66, and persons over the age of 45 are most likely to develop it. According to the American Cancer Society, widespread screening of adults over 50 and the removal of pre-cancerous growths known as polyps are contributing to a decline in colorectal cancer occurrences and deaths in older people.
Those under 45 have a low chance of developing colorectal cancer, the number of cases and fatalities in this age group has been rising since the 1990s.
Currently, a research of American veterans has identified certain elements that are linked to a higher risk of early-onset colorectal cancer in males. The authors contend that in some situations, targeted screening may aid in case prevention.
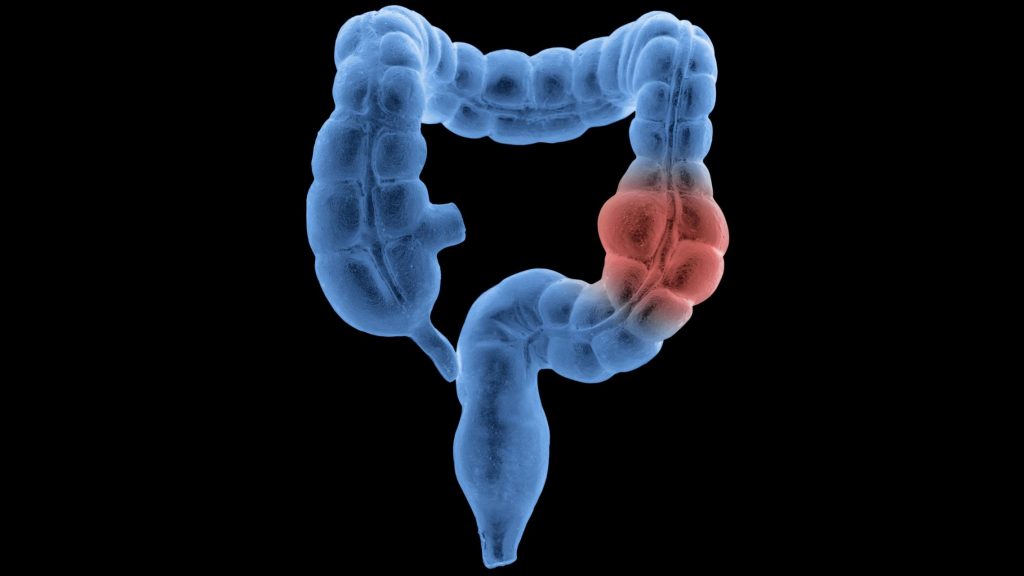
What exactly is colorectal cancer?
Cancer that starts in the colon or rectum is called colorectal cancer. These cancers may also be known as colon cancer or rectal cancer depending on where they first appear.
The majority of colorectal malignancies begin as polyps, which are growths on the colon’s inner lining. Even though not all polyps develop into cancer, some of them can over time.
In the United States, colorectal cancer ranks third among all cancers, excluding skin cancer, according to the American Cancer Society.
Causes of colorectal cancer risk
The researchers located 956 men between the ages of 35 and 49 who had received a non-hereditary colorectal cancer diagnosis between 2008 and 2015 from the National Veterans Affairs database in the United States. 600 of them satisfied the requirements for study inclusion.
These were then matched with 1,200 controls who underwent colonoscopies but did not develop colorectal cancer and 1,200 controls who had not.
For both cases and controls, the researchers examined sociodemographic and lifestyle characteristics, family and personal medical histories, physical measurements, vital signs, medications, and laboratory results. For people with colorectal cancer, data from the six to eighteen months before diagnosis were utilized to identify characteristics that might vary with the development of the disease.
Age, cohabitation, employment, BMI, malignancies in first- or second-degree relatives, comorbidities, alcohol use, hyperlipidemia, and usage of statins, non-steroidal anti-inflammatory medications (NSAIDs), or multivitamins were all examined to find risk variables.
From this, scientists discovered 15 variables that were each independently linked to a higher chance of developing colorectal cancer at an early stage. They singled out seven of these that offered equivalent precision and whose data are easily obtainable:
- elder age (between the ages of 35 and 49)
- NSAIDs (such as aspirin or ibuprofen) should not be regularly used.
- no consistent statin use
- usage of alcohol today
- relatives in the first or second degree who have colorectal cancer
- a greater burden of sickness
According to corresponding author Dr. Thomas F. Imperiale, a research scientist at the Regenstrief Institute, several characteristics raised risk more than others:
It was more significant to have a first- or second-degree family who had colorectal cancer. Non-steroidal anti-inflammatory drug use and statin use were two additional factors with a stronger impact.
Risk of colorectal cancer and lifestyle
The risk of colorectal cancer may be increased by a number of lifestyle variables, according to the Centres for Disease Control and Prevention (CDC). These consist of:
- absence of frequent exercise
- consuming little fruit and veg
- A diet that is high in processed meats or low in fibre and high in fat
- Obesity and overweight
- drinking alcohol
- nicotine use
The study’s author, Dr. Bilchik, who was not involved in it, emphasized the importance of lifestyle factors:
According to this study, lifestyle choices have a significant impact on the development of colorectal cancer. For instance, taking statins is connected to elevated cholesterol, and food and alcohol have also been linked to a number of different cancers.
Screening for high-risk individuals
The researchers pointed out that although their study only included men, men are still twice as likely to develop colorectal cancer as women of any age. However, they are currently conducting research along these lines on female risk factors.
They emphasised that not all younger men should have colorectal cancer screenings, but those who are at higher risk may benefit.
“Only high-risk men between the ages of 35 and 44 should be screened. Guidelines now recommend colorectal cancer screening for men between the ages of 45 and 49 but do not specify how (i.e., which test),” Thomas F. Imperiale, M.D.
“The risk factors may be helpful in deciding whether noninvasive testing (with the faecal immunochemical test or with the multi-target stool DNA test) or a colonoscopy is more appropriate,” Dr. Imperiale said to us.
Additionally, he hoped that highlighting these risk factors will prompt males between the ages of 45 and 49 who are already eligible for screening to request testing.
The findings indicating that colorectal cancer screening is advised starting at age 45 are particularly pertinent to male veterans under the age of 35. Dr. Imperiale continued, “However, the results may also be valuable for persuading 45-49 year old male veterans that they should be examined.
How is colon cancer identified?
Your doctor would advise exams and testing to determine the cause if you have colorectal cancer symptoms or if a screening test result was abnormal.
The American College of Physicians advises colorectal cancer screening using one of the following methods for those with a typical risk of developing the disease:
- a colonoscopy every ten years
- every two years, a high sensitivity guaiac-based faecal occult blood test (gFOBT) or faecal immunochemical test (FIT)
- FIT every two years in addition to flexible sigmoidoscopy every ten years.
People who have a higher risk of developing colorectal cancer should discuss the type and frequency of screening that is most appropriate for them with their doctor.
To determine your personal risk level, use this risk calculator. Additional testing is necessary to stage colorectal cancer and determine the best course of therapy if it is discovered.
Physical examination and medical history
To ascertain whether you have any risk factors, such as a family history of colorectal cancer, your doctor will inquire about your medical history. Additionally, the duration of your symptoms will be questioned of you.
During a physical examination, your abdomen will be felt for lumps or enlarged organs, and a digital rectal exam (DRE) may be performed.
A gloved finger is inserted into your rectum by the doctor during a DRE to look for any anomalies.
Stool tests
Tests to look for blood in your stool may be advised by your doctor. To the naked eye, blood in the faeces is not always obvious. These examinations aid in finding blood that cannot be seen.
These tests, such as a FOBT or FIT, are carried out at home with the aid of a kit that is provided. You can use the kit to gather one to three stool samples for testing.
A blood test
Blood tests may be required to look for colorectal cancer symptoms include anaemia, which is a condition when there are not enough red blood cells in the body.
Additionally, your doctor can request tests for liver function and tumour markers such carcinoembryonic antigen (CEA) and CA 19-9. Colorectal cancer cannot be identified by blood testing alone.
Signoidoscopy
Your doctor can view the interior of your sigmoid colon via a sigmoidoscopy, also known as a flexible sigmoidoscopy. If a colonoscopy is not possible for any reason, this less intrusive technique could be suggested instead.
Colonoscopy
A diagnostic colonoscopy is carried out as a result of symptoms you are experiencing or an anomaly discovered during a screening test. The test is performed to observe your colon and rectum in their entirety.
A colonoscope, which is put into the body through the anus, is used to perform it because it is a small, flexible tube with a camera on the end.
The colonoscope can be used to insert specialised tools that can be used to remove polyps and collect tissue samples for biopsies.
Proctoscopy
During a proctoscopy, the anus is used to introduce a proctoscope. To observe the interior of the rectum, a proctoscope is a short, rigid tube with a camera at one end. It is used to examine the rectum for cancer.
Biopsy
A biopsy is a lab test that looks at a tissue sample. Polyps or questionable spots are typically removed during a colonoscopy, but if necessary, they can also be removed surgically.
The tissue is delivered to a lab where a microscope is used to examine it. The samples might also be examined for gene alterations if cancer is discovered. To help categorise the malignancy, more lab tests could be carried out.
Imaging exams
Imaging examinations can:
- view potential cancerous regions that are suspicious
- determine the extent of the cancer’s spread
- test the efficacy of the treatment
REFERENCES:
- https://www.medicalnewstoday.com/articles/colorectal-cancer-earlier-screening-should-be-considered-for-young-men-at-high-risk
- https://www.healthline.com/health/colorectal-cancer/colorectal-cancer
- https://www.mdanderson.org/cancerwise/why-are-more-young-adults-getting-colorectal-cancer-what-to-know.h00-159385890.html
- https://www.cancer.net/cancer-types/colorectal-cancer/screening
For Cancer disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=10