The importance of the stomach in Parkinson’s research.
There is presently no cure for Parkinson’s disease, which affects millions of people worldwide. The specific etiology of this disorder is still unknown. Some academics are now focusing on the gut to comprehend the underlying mechanics. Why, and what might this study show? In this episode of our podcast In Conversation, we talk about how Parkinson’s disease may be influenced by gut health.
Parkinson’s disease is a neurological condition that affects mobility, balance, and muscle control in millions of people worldwide. However, it can also cause mood changes, digestive problems, a decline in memory and other cognitive abilities, and other symptoms.
The World Health Organisation (WHO) reports that the prevalence of Parkinson’s disease has doubled globally over the past 25 years and that the condition has caused “5.8 million disability-adjusted life years” globally.
Some of the current treatments for Parkinson’s disease include dopaminergic medications, deep brain stimulation, speech, and occupational therapy, but researchers are always looking for new and improved therapies.
Researchers are working to gain a better understanding of the mechanisms underlying Parkinson’s disease to pave the path for more effective treatments.
In the last 12 months, several research have concentrated on one specific element of Parkinson’s disease, particularly gut health. But why, and what insights may it provide into Parkinson’s, can gut health provide?
In the most recent episode of our In Conversation podcast, we welcomed two guests: Dr. Ayse Demirkan and Gary Shaughnessy, to learn more about the most recent research and how the disease can affect particular people.
Why trust your gut?
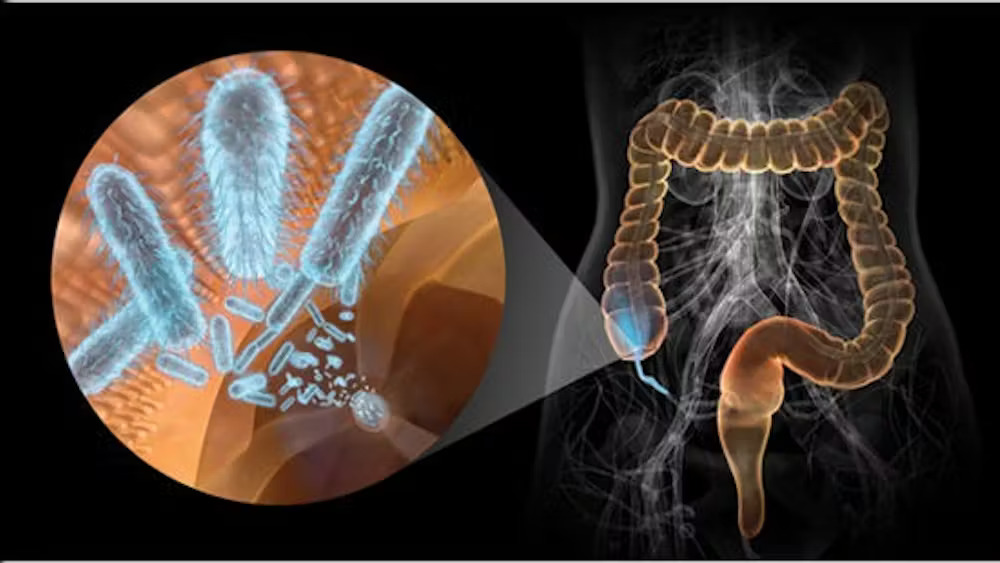
There has been a growing body of research over the past few years suggesting that the brain and the gut are capable of two-way communication. This is known as the gut-brain axis by researchers.
The gut-brain axis has been linked to a variety of brain-related illnesses, including depression and dementia. And while the relationship between the gut and the brain may be less obvious in other disorders, it is actually more evident in Parkinson’s disease, which is also sometimes accompanied by gastrointestinal symptoms like constipation.
The Braak hypothesis is one view on Parkinson’s disease. According to a reliable source, there are typically two ways for an unknown infection to enter the brain, one of which involves the gut.
The vagus nerve, the longest cranial nerve that connects the brain to, among other organs, the intestines, may be one route by which pathogens enter the body, travel through the gut, and then advance to the brain. Parkinson’s disease may then start to manifest as a result of this.
In our podcast, Dr. Demirkan recognized that it may initially seem strange to think about using your gut to learn more about Parkinson’s disease, but that the Braak hypothesis offers an intriguing lens through which to examine potential underlying mechanisms.
“Through the Braak hypothesis, there comes the idea that the disease actually starts in the intestines, and then through the vagus nerve, it spreads to the other tissues, and towards the brain,” she said.
She claims that for one straightforward reason alone, Parkinson’s disease is the neurological disorder that is most intriguing to examine regarding gut health because its gut microbiome stands out the most.
Parkinson’s disease has a distinct gut microbiota.
Dr. Demirkan and her colleagues recently discovered that people with Parkinson’s disease have unique gut microbiomes that were characterised by dysbiosis, the phenomenon of imbalance between so-called good and bad bacteria.
According to their research, those with Parkinson’s disease have gut flora that is different from those who do not have it by about 30%.
Dr. Demirkan stated in the podcast that “we found one-third of these microbes in the gut of people with Parkinson’s disease to be different.”
“As a result, this strongly suggests dysbiosis. Also different were the bacteria’s modes of operation and the types of genes they possessed. We observed a decrease in the number of short-chain fatty acid manufacturers, such as gut-friendly bacteria. Escherichia coli and other harmful bacteria were identified in greater numbers, and numerous bacterial pathways were disrupted, which may have an impact on the health of the neuronal tissues,” according to Dr. Ayse Demirkan.
In the guts of Parkinson’s disease patients, Dr. Demirkan and her colleagues discovered that levels of bacteria like Bifidobacterium dentium, which can result in infections like brain abscesses, were noticeably raised.
Desulfovibrio bacteria may be related to Parkinson’s disease, according to research from the University of Helsinki that was published in the May 2023 issue of Frontiers. These microorganisms release hydrogen sulfide, which can cause different types of inflammation.
Desulfovibrio was mentioned in another study from The Chinese University of Hong Kong that was published in Nature Communications in May 2023. This study found an “overabundance” of these bacteria in persons with REM sleep behavior disorder and early Parkinson’s disease indicators. The goal of the study was to find a way to diagnose Parkinson’s disease earlier.
What potential mechanisms exist?
The question that arises is: What mechanisms might mediate gut bacteria’s impact on neurological health, assuming that they do in fact contribute to Parkinson’s disease?
Given that some of the bacteria that are overabundant in this condition are pro-inflammatory, which means they can cause inflammation, one theory raised in the studies on the connection between the gut and the brain in Parkinson’s is that systemic inflammation may be one of the processes involved.
Research reveals that immunosuppressant medicine may reduce the chance of Parkinson’s disease, which raises the possibility that a medication of a similar kind may potentially assist manage the disease.
Parkinson’s disease is characterised by chronic brain inflammation, and some studies appear to suggest that systemic inflammation may exacerbate chronic brain inflammation and speed up the course of the disease.
In fact, some inflammatory disorders have been associated with an increased risk of Parkinson’s. For instance, a 2018 Danish study found that those with inflammatory bowel disease (IBD) had a 22% higher chance of developing Parkinson’s disease than their non-inflammatory counterparts.
In the podcast, Dr. Demirkan concurred that “bad” bacteria in the stomach may be the source of inflammation associated with Parkinson’s disease. She emphasised that more investigation is required before drawing clear conclusions because this proposed mechanism is not yet established.
Could nutrition help Parkinson’s patients with dysbiosis?
It could be logical to assume that nutrition could aid in the fight against gut dysbiosis and perhaps offer a simple option for symptom treatment if gut bacteria may play a role in Parkinson’s disease.
While there are certain dietary suggestions and nutritional supplements that may help some people with symptom alleviation, it’s still not clear how much food can actually do to change how this condition develops.
According to one study from 2022, diets rich in flavonoids, which are natural pigments present in many fruits, may be associated with a lower risk of mortality from Parkinson’s disease.
Additionally, an earlier study from 2018 suggested that a protein called parvalbumin, which is present in many types of fish, may help prevent Parkinson’s disease by preventing alpha-synuclein from clumping together in the brain, which occurs in the brains of people with Parkinson’s and disrupts signals between brain cells.
Dr. Demirkan did, however, show some scepticism when asked about the ability of food and vitamins to control gut flora in Parkinson’s patients.
She emphasised that it is challenging to provide generic advice that would truly be useful because different persons have various risk factors for Parkinson’s as well as varied forms of the disease.
“I find it very challenging to offer advice to anyone because each of us has a unique gut microbiota. Therefore, I believe that preventing the condition is one thing and that long-term maintenance, along with the various consequences of the disease, is another. I can’t really offer any advice because of this, although research indicates that consuming more sugar is problematic.
Can exercising treat Parkinson’s disease?
Nevertheless, some evidence suggests that exercising can help people with Parkinson’s disease manage their symptoms.
According to a study from 2022 that was published in Neurology, those with early-stage Parkinson’s disease may benefit from regular, moderate-to-vigorous exercise since it can delay the disease’s progression.
According to research published in 2017, doing at least 2.5 hours of exercise each week can assist Parkinson’s patients become more mobile while also delaying the onset of the disease.
Dr. Demirkan concurred that using exercise as a management tool for Parkinson’s disease can be beneficial. Exercise by itself is a fantastic technique to mould our brain and body, she claimed.
“There are some significant physiological consequences that we can consider in terms of reversing [Parkinson’s] disease. Your body must endure a lot of stress when you run a marathon, for instance. For instance, you may notice that your body temperature rises steadily and in a feverish manner. One thing is that there is a long-term rise in core heat, and it should unquestionably have a significant impact on the stomach,” she said.
In fact, some study indicates that the heat stress experienced during exercise may decrease intestinal blood flow, which may ultimately have an impact on the gut microbiota by allowing for the expansion of some bacteria while suppressing others.
In terms of the optimum type of exercise for persons with Parkinson’s disease, a Cochrane study that was released in January 2023 came to the conclusion that pretty much all types of exercise can assist those with this illness to live better lives. The authors of the review state that the available evidence “probably has a large beneficial effect” on the quality of life of aqua-based training.
REFERENCES;
- https://www.medicalnewstoday.com/articles/in-conversation-why-parkinsons-research-is-zooming-in-on-the-gut
- https://pubmed.ncbi.nlm.nih.gov/37298727/
- https://journals.physiology.org/doi/full/10.1152/ajpgi.00058.2020
- https://www.nature.com/articles/s41531-020-0112-6
For Parkinson’s disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=64