Can consuming red meat really cause you cancer?
Years have been spent by nutritionists and health professionals arguing the advantages and disadvantages of consuming red meat in an effort to discover whether it is beneficial or harmful to health. Results have been inconsistent so far.
Red meat, according to researchers, supplies vital elements like protein, vitamin B-12, and iron. Yet, research indicates that consuming large amounts of red meat may increase one’s risk of developing some malignancies, heart disease, and other illnesses.

The amount of red meat that may be healthy is examined in this article along with what the science and official dietary recommendations have to say.
The effects of red meat on health are the main topic of this essay. The ethical and environmental concerns surrounding the consumption of red meat are not addressed.
Is red meat nutritious?
Iron, vitamin B-12, and zinc are among the healthy components found in red meat.
The primary nutritional sources of vitamin B-12 are animal-based foods like meat and dairy. Because of this, individuals who consume a vegetarian or vegan diet may need to supplement their B-12 to avoid developing B-12 deficiency anaemia.
The United States Department of Agriculture reports that one 3.5-ounce (oz) or 100-gram (g) serving of raw ground beef provides the following nutrients:
- calories in 247
- Fat weight 19.07 g
- Protein content: 17.44 g
- Iron 1.97 milligrammes (mg)
- Potassium 274 mg
- zinc 4.23 mg
- B-12 vitamin dosage of 2.15 micrograms
A piece of meat’s nutritional value might vary depending on a variety of circumstances. The amount of calories and fat, for instance, differs between cuts from various animal parts. The food of the animal, how the farmer grew the animal, and even the animal’s age and sex can have an impact on the nutritional value of the meat.
Several varieties of red meat are recommended as good sources of heme iron by the National Institutes of Health (NIH). The only foods that contain heme iron are meat, poultry, and shellfish. Plants and meals enriched with iron, such as cereals and plant milk, contain nonheme iron.
Heme iron is more bioavailable, which implies that the body can utilise it more readily, according to the NIH. Despite the fact that many people consume adequate amounts of iron, the NIH notes that some people are at risk of iron deficiency, including:
- infants
- little children
- those with frequent menstruation
- expecting mothers
Difference between unprocessed and processed red meat
It’s crucial to comprehend the many varieties of red meat before delving into the studies on the connection between red meat and cancer.
Unprocessed
Red meats that haven’t been altered or manipulated are known as unprocessed red meats. Examples comprise:
- steak
- Lamb chops
- lamb ribs
Unprocessed red meat can be healthy on its own. It frequently contains high levels of protein, vitamins, minerals, and other vital components. When processed, red meat loses some of its original value.
Processed
Meat that has undergone some sort of modification—often for taste, texture, or shelf life—is referred to as processed meat. Meat that has been salted, cured, or smoked can accomplish this.
Red meats that have been processed include:
- hotdogs
- the salami and pepperoni
- ham with bacon
- dinner meats
- sausage
- bologna
- jerky
- cans of meat
Processed red meat typically has fewer healthy elements and is higher in fat and salt than unprocessed red meat. When taken in large quantities, red meat is regarded by experts as a potential cause of cancer. Processed meat and the chance of developing cancer are more closely related.
Processed meat has been identified as a carcinogen by experts. As a result, its link to cancer is now established.
What the research says
Many studies have examined the link between eating unprocessed and processed red meat and health outcomes over time.
There is some evidence that eating a lot of red meat may increase your chance of developing some malignancies, while the data are still conflicting.
IARC methodology
A division of the World Health Organization is the International Agency for Research on Cancer (IARC). It is made up of professionals from throughout the world who work to categorise potential carcinogens (cancer-causing agents).
IARC members analyse scientific papers regarding a potential carcinogen for several days when there is a lot of evidence to suggest that it may cause cancer.
They take into account many aspects of the data, such as how people and animals react to a potential carcinogen and how cancer might grow following exposure to it.
The classification of the probable carcinogen according to its propensity to cause cancer in humans is one step in this procedure.
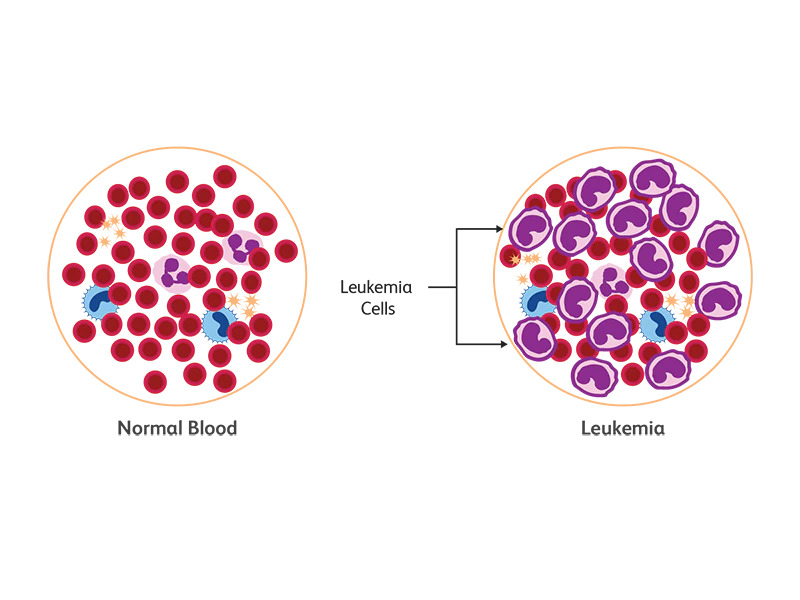
Group 1 agents are those that have been shown to cause cancer in people. On the other hand, group 4 agents consist of substances that most likely do not cause cancer.
Remember that this classification does not indicate the risk a carcinogen poses. It simply shows the amount of data that supports the association between particular carcinogens and cancer.
IARC conclusions
22 specialists from ten different countries gathered in 2015 to assess the body of knowledge regarding the connection between red meat and cancer.
Almost 800 studies over the previous 20 years were reviewed. Just processed or unprocessed red meat was the focus of certain investigations. Others observed them both.
To reduce cancer risk, avoid processed meat
Avoid eating processed meats if you want to lower your risk of colorectal cancer and perhaps other cancers as well.
Processed meat is a Category 1 carcinogen, according to the IARC. In other words, there is sufficient study to demonstrate its link to human cancer. Here are some additional Group 1 carcinogens for context:
- tobacco
- ultraviolet rays
- alcohol
Once more, the basis for this classification is the evidence that links a certain agent to cancer. Although there is compelling evidence that all Group 1 agents cause cancer in humans, not all of them necessarily carry the same degree of risk.
For instance, when it comes to the danger of developing cancer, eating a hot dog isn’t necessarily equivalent to smoking a cigarette.
Be mindful about red meat consumption
For many people, unprocessed red meat is a crucial component of a healthy diet. It provides ample amounts of:
- protein
- vitamin B-6 and vitamin B-12
- minerals, such as selenium, iron, and zinc
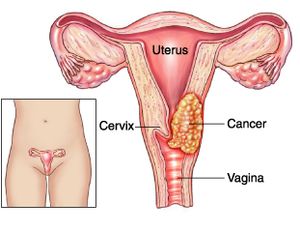
Yet, the IARC analysis came to the conclusion that frequently consuming red meat probably raises the risk of developing several malignancies.
Therefore, there’s no need to exclude all red meet from your diet. Simply be mindful of how you prepare it and how much you consume.
Cooking techniques
In their analysis, IARC specialists also mentioned that the manner red meat is prepared can affect your chance of developing cancer.
High-temperature meat grilling, burning, smoking, or cooking appears to enhance risk. But, the IARC specialists stated that there wasn’t enough data to issue any official advice.
Serving suggestion
There is no requirement to completely give up unprocessed red meat, according to the authors of the IARC analysis. So it’s recommended to stick to three servings per week.
The bottom line
Red meat has come under fire for its alleged associations with a number of diseases, including cancer. According to experts, routinely consuming red meat may up your risk of developing colorectal cancer.
A consensus among experts also exists that consuming a lot of processed meat does raise your chance of developing cancer. Therefore, you don’t have to completely eliminate red meat from your diet. Just make an effort to stick to eating only a few servings of high-quality, unprocessed red meat per week.
REFERENCES:
- https://www.healthline.com/health/does-red-meat-cause-cancer
- https://www.medicalnewstoday.com/articles/326156
- https://www.wcrf.org/diet-activity-and-cancer/risk-factors/meat-fish-dairy-and-cancer-risk/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4144110/
For more details, kindly visit below.