Daily exercise of just 20 to 25 minutes may reduce the risk of death from extended sitting.
The higher risk of death linked to a sedentary lifestyle can be eliminated with about 22 minutes of moderate to intense physical activity every day, according to a recent study. People’s risk of dying reduces more the more they exercise. The results of the study demonstrate that regular exercise can be done in one sitting or in smaller bursts during the day. Contrary to popular belief, a recent study indicates that much less exercise can lower a person’s risk of death. The study discovers that a sedentary lifestyle can lower one’s chance of dying young by as much as 22 minutes per day of moderate to vigorous physical activity (MVPA).
Naturally, the benefits of exercise are dose-dependent, meaning that, up to a certain degree, the more activity, the lower the risk of mortality. 11,989 participants in multiple fitness-tracker studies—the Swedish Healthy Aging Initiative, the Norwegian National Physical Activity Survey, the Norwegian Tromso Study, and the U.S. National Health and Nutrition Examination Survey—were monitored by the study’s authors. Every participant in the studies, who was at least fifty years old, gave the researchers information about their height, weight, sex, education, alcohol and smoking habits, and history of diabetes, heart disease, or cancer. 6,042 people sat for 10.5 hours or more every day, compared to 5,943 participants who sat for less than that amount. The purpose of the study was to evaluate the impact of physical activity and inactive time on mortality risk as determined by death registries. If an individual does not exercise for more than 22 minutes per day, sitting for more than 12 hours per day is linked to a 38% higher risk of death than sitting for 8 hours.
A minimum of 75 minutes of intense activity, 150–300 minutes of moderate–to–vigorous exercise per week, or a combination of both is advised by the World Health Organization (WHO).
The first author of the study, Dr. Edvard H. Sagelv of UiT The Arctic University of Norway in Tromso, stated: “There is some disagreement in the research community regarding the dangers of prolonged periods of inactivity. Sedentary time is not that harmful when compared to not exercising, in my opinion. He continued, “Yet prior research suggests that prolonged periods of inactivity are elevating the likelihood of illness and untimely demise.”
“Our legs and core muscles will weaken if we’re not using them, which will make it harder for us to walk a little distance, which will decrease our desire to be active,” she continued. Additionally, this raises the possibility of falling, which increases our risk of injuries that further discourage us from engaging in physical activity. “Keep in mind that the heart is a muscle,” Dr. Zaslow advised. She pointed out that the cardiac muscle weakens with less activity, making physical activity much more difficult as the heart must be reconditioned. According to Dr. Zaslow, cardiometabolic illness has been linked to sedentary lifestyles.
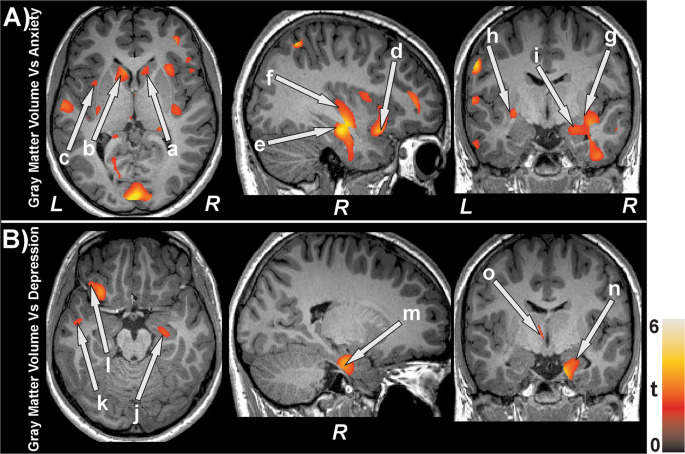
Dr. Melody Ding, who was not involved in the study, stated that although the study is focused on older adults, physical activity is known to give a range of advantages, including mental health, cardiometabolic profiles, and cognitive functioning. Dr. Ding stated, “There are good reasons to be active throughout your lifespan.” Dr. Zaslow made the point that exercise is necessary for even young children to develop and strengthen their muscles since it prepares them for a lifetime of physical activity. Furthermore, physical activity is linked to improved mental health, including a decrease in anxiety and depression. This is still another significant advantage, according to Dr. Zaslow, considering the highly publicized mental health issue among youth.
She said that exercise helps people sleep better as well, making it easier to fall asleep and stay asleep longer. “We are aware that injury rates are lower when we get better sleep. Thus, research indicates that children who get more than eight hours of sleep have 50% fewer injuries. “I consider exercise and exercising consistently to be like an upward spiral,” Dr. Zaslow remarked. Dr. Sagelv emphasized that the study’s 22 minutes of daily physical exercise equates to the 150 minutes that the WHO recommends. According to our research, people who engage in moderate-to-intense physical exercise for longer than 22 minutes a day do not have a higher risk of dying from being inactive for longer. This runs counter to the WHO’s guideline, according to him, to deal with high sedentary time that cannot be avoided by consuming more than 150–300 minutes of MVPA each week.
It doesn’t seem to have an upper limit at which it stops being beneficial to health. The risk decrease does however, seem to level off at the higher ends, roughly 60–120 minutes per day, especially for people who are extremely sedentary.” It’s also not necessary for people to engage in 22 minutes of action all at once every day, as per Dr. Zaslow and earlier studies. Taking ten or fifteen minutes here and there to engage in “exercise snacking” may be a more manageable task for individuals with hectic schedules. It’s crucial to keep in mind that, from the standpoint of public health, performing any MVPA is preferable to performing none at all. Dr. Ding stated that it is better to exert a little bit more effort even if one is unable to meet the goal.
REFERENCES:
https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/exercising-just-for-20-25-minutes-can-prevent-death-risk-due-to-prolonged-sitting/articleshow/104784810.cms?from=mdr
https://www.medicalnewstoday.com/articles/daily-20-25-mins-of-physical-activity-may-offset-death-risk-from-prolonged-sitting
https://www.bmj.com/company/newsroom/daily-20-25-mins-of-physical-activity-may-offset-death-risk-from-prolonged-sitting/
For any medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com