Consequences of ignoring the vaccination of rotavirus.
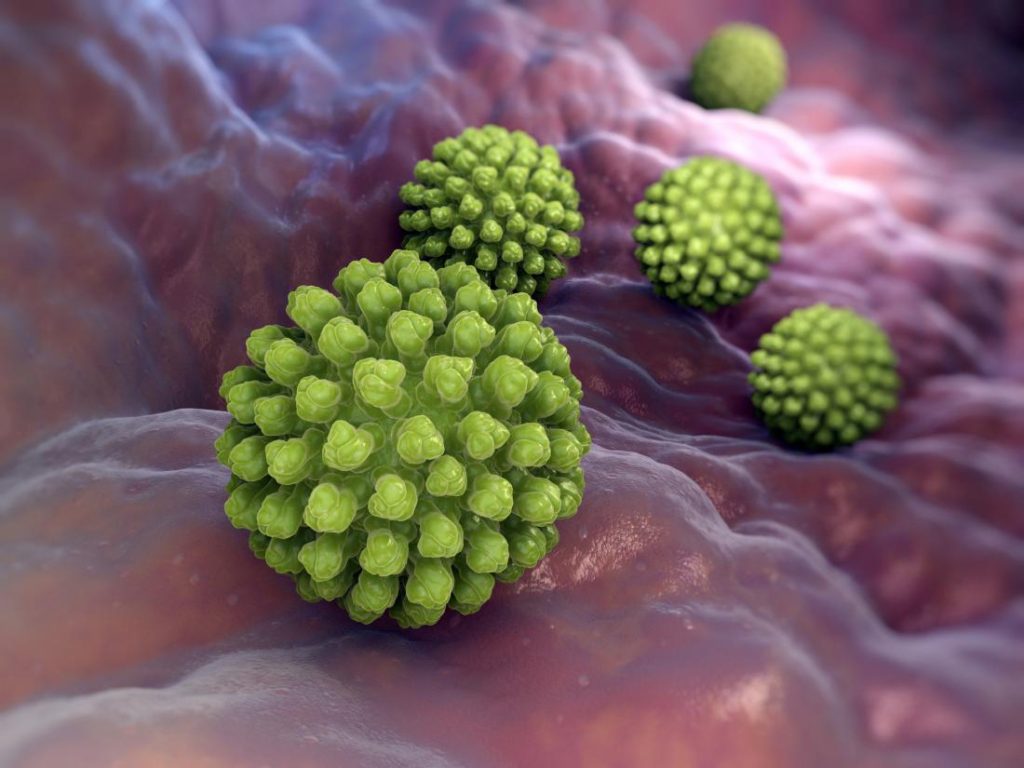
What Is Rotavirus?
Children under the age of five are especially susceptible to rotavirus infections. It spreads quickly and is caused by a virus that is simple to spread. Adults can get the infection, though it normally isn’t as serious as it is in youngsters, who tend to have it more frequently.
The following annual statistics for children aged 5 and under in the United States were caused by the infection prior to the introduction of the rotavirus vaccination in 2006, according to the Centers for Disease Control and Prevention (CDC):
- 400 000 paediatrician appointments
- 70,000 to 55,000 hospitalisations
- at least 200,000 trips to the emergency room
- from 20 to 60 fatalities
When it comes to preventing serious rotavirus disease, the vaccine is more than 90% effective.
Medication is not used to treat rotavirus. In most cases, it gets better on its own over time. Dehydration, on the other hand, is a major worry. To avoid problems that could be life-threatening, it is crucial to know when to seek medical help.
Symptoms of rotavirus
Normally, two days after rotavirus exposure, an illness develops. Fever and vomiting are the initial symptoms, which are followed by watery diarrhoea that lasts three to seven days. Additionally, the infection may result in stomach ache.
A rotavirus infection in healthy people may not show any symptoms at all or only show mild ones.
- Vomiting, fever, and stomach discomfort. These symptoms normally appear in the beginning of rotavirus and then subside.
- After the first three symptoms have subsided, diarrhoea starts. The diarrhoea may persist for 5 to 7 days as the virus makes its way through your child’s body.
In the event that your child:
- Lethargy
- repeated vomiting
- less thirst for fluids
- stools that are dark, have blood or pus in them
- Any fever in a baby under the age of six months
- a child older than 6 months who has had a high temperature for more than 24 hours
Your youngster might not feel like eating or drinking due to all the vomiting and diarrhoea. They may become so dehydrated that it poses a serious risk to their lives. Dehydration is a risk factor for older persons, particularly those with additional illnesses or disorders.
If you experience any of these signs of dehydration, contact your doctor right away:
- Anxiousness
- Crying while not crying
- Dry diapers or infrequent urination
- Dizziness
- throat and mouth are dry
- extreme drowsiness
- light skin
- recessed eyes
Adults with rotavirus
Adults may also suffer certain rotavirus symptoms, including:
- vomiting
- acute exhaustion
- an extreme fever
- irritability
- dehydration
- abdomen ache
Many healthy individuals, however, only feel them to a lesser extent. Adults with rotavirus may even go weeks without showing any symptoms.
Rotavirus Causes and Risk Factors
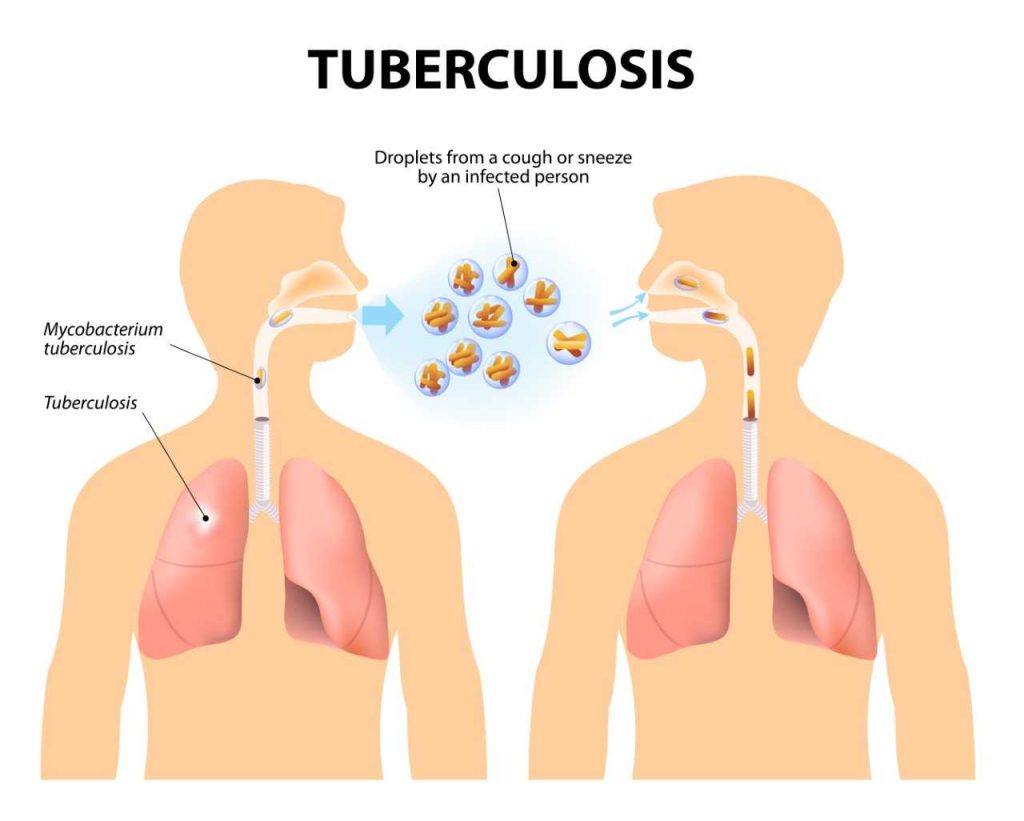
When hands are not thoroughly cleansed after using the restroom or changing a diaper, rotavirus bacteria that are present in a person’s faeces (poop) can travel to other surfaces. Fecal-oral transmission occurs when these bacteria come into contact with a mouth.
Rotavirus can spread even in the absence of symptoms. Rotavirus can affect anyone, however it usually has an impact on:
- Infants
- little children
- nearest relatives
Those who take care of children, such nannies or daycare providers. If your child has rotavirus, it can be found in their poop up to 10 days before their symptoms start to fade. Rotavirus can spread to your child’s hands during the time when they wipe their hands after using the restroom. They risk contaminating everything they touch if they don’t wash their hands, which include:
- Markers and crayons
- Food
- surfaces like kitchen countertops and sinks
- toys, including consoles and shared electronics like iPads
- Utensils
- Water
You risk contracting an infection if you contact your child’s unwashed hands or any other contaminated object before touching your mouth. Cleaning is essential. Rotavirus can survive for weeks on surfaces and objects.
Rotavirus vaccines
In 2006, the rotavirus vaccination was first made available. Before this, at least one episode of rotavirus infection in early children was typical. Rotavirus-related hospitalisations and fatalities have drastically decreased since the vaccine’s introduction.
Make sure your child receives the necessary vaccinations to help avoid rotavirus and its complications. There are two types of the vaccine:
- Rotarix: two doses given to infants at 2 and 4 months
- RotaTeq: 3 doses given at 2, 4, and 6 months of age
Both of these vaccinations are oral, which means they are given orally rather than intravenously. Adults and older children cannot get the immunisation. This is why medical specialists advise getting your child the rotavirus vaccine as soon as possible.
No vaccine is 100% effective, even though it virtually always shields against serious cases of illness from rotavirus. Your paediatrician can help you decide whether this particular vaccine is the appropriate preventive approach for your kid based on the risks and benefits involved.
Infants who have severe intussusception or combined immunodeficiency, as well as those who are already very unwell, shouldn’t receive the vaccine. A few infrequent vaccination adverse effects are as follows:
- diarrhea
- fever
- fussiness
- irritability
- Having an intestinal obstruction called intussusception can result in severe stomach pain, vomiting, and bloody faeces (this is very rare)
REFERENCES:
- https://www.healthline.com/health/rotavirus
- https://www.webmd.com/children/guide/what-is-rotavirus
- https://my.clevelandclinic.org/health/diseases/8275-rotavirus
- https://www.mayoclinic.org/diseases-conditions/rotavirus/symptoms-causes/syc-20351300
For more details, kindly visit below.