Quick peek on causes and symptoms of Hypothyroidism.
Thyroid
When the thyroid does not produce and release enough thyroid hormone into your bloodstream, it is known as hypothyroidism. Your metabolism becomes slower as a result. Hypothyroidism, also known as an underactive thyroid, can make you feel exhausted, put on weight, and have trouble handling cold weather. Hormone replacement therapy is the primary method of treatment for hypothyroidism.
What is hypothyroidism?
When your body doesn’t create enough thyroid hormones, hypothyroidism develops. The thyroid is a little gland with a butterfly form that is located in front of the windpipe. Hormones that aid in energy regulation and use are released.
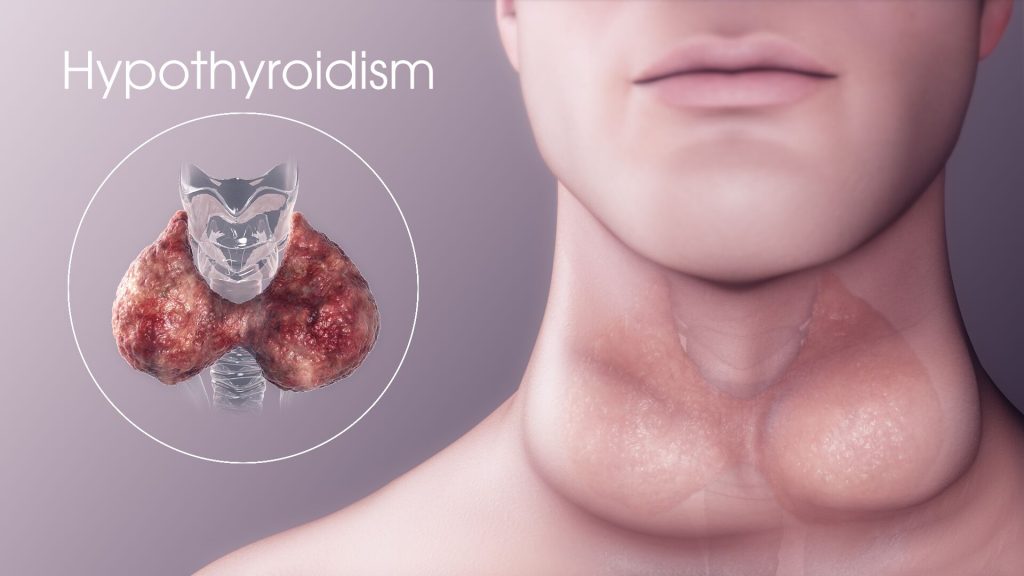
The actions of your digestive system and your heartbeat are among the processes that thyroid hormones assist regulate. The natural processes of your body slow down if you don’t have enough thyroid hormones.
Hypothyroidism, often known as an underactive thyroid, typically affects adults over 60 and is more prevalent in women than in males. After symptoms appear or during a regular blood test, it might be identified.
The term used to describe an early, mild version of the illness is subclinical hypothyroidism. It’s crucial to understand that treatment for hypothyroidism is regarded as straightforward, secure, and efficient if you have lately obtained a diagnosis.
The majority of treatments focus on adding synthetic hormones to your low levels of natural hormones. These hormones will take the place of those your body isn’t manufacturing on its own and assist in restoring normal bodily processes.
How common is hypothyroidism?
The condition of hypothyroidism is pretty typical. Nearly 5% of Americans between the ages of 12 and 60 suffer with hypothyroidism.
With age, the disease becomes increasingly prevalent. It strikes more commonly in people over 60. The prevalence of an underactive thyroid is higher in women. Actually, 1 in 8 women will experience thyroid problems.
Signs and symptoms of hypothyroidism
The physical symptoms of hypothyroidism frequently range between individuals and might be challenging to pinpoint. The timing and severity of the signs and symptoms are also influenced by the condition’s severity.
Fatigue and weight increase are two early signs. Note that regardless of how well your thyroid is functioning, these both grow more prevalent as you age. As a result, you might not identify these changes as thyroid-related until additional symptoms manifest. For instance, these could include the scaly, rough, and dry skin and brittle nails linked to hypothyroidism.
The most typical hypothyroidism warning signs and symptoms are generally as follows:
- fatigue
- gaining weight
- depression
- constipation
- being chilly
- reduced perspiration
- reduced heartbeat
- increased cholesterol levels
- arid skin
- thinning, dry hair
- a weakened memory
- muscular tremor
- stiffness, pains, and tightness in the muscles
- joint discomfort and stiffness
The majority of persons experience a slow progression of symptoms over many years. The signs may be easier to spot when the thyroid slows down more and more. Naturally, many of these symptoms also increase in frequency as we age.
Consult your doctor if you think a thyroid issue is the cause of your symptoms. To find out if you have hypothyroidism, they can ask for a blood test.
Symptoms of hypothyroidism in adulthood
Research suggests that in addition to the most typical hypothyroidism symptoms, men may also experience erectile dysfunction.
Additional signs of hypothyroidism in women include:
- fertility problems
- menstrual changes, especially erratic or excessive bleeding
- pregnancy-related issues, such as anaemia
Hypothyroidism can also manifest themselves while a woman is pregnant. Typically, hypothyroidism symptoms are consistent with other hypothyroidism patients.
Young individuals with hypothyroidism
Younger people are less likely to develop hypothyroidism, but it is still possible. Children with the syndrome may develop more slowly, while teenagers with it may have early puberty.
Congenital hypothyroidism, which refers to a lack of thyroid function at birth, is another possibility. Infants with hypothyroidism may exhibit the following signs:
- more sleep than normal
- constipation
- difficulty with feeding
- sluggish growth (if the condition is untreated)
Babies with hypothyroidism occasionally don’t exhibit any symptoms.
Severe signs of hypothyroidism
If hypothyroidism is not addressed, other symptoms could appear:
- sensitive, swollen face
- hoarseness
- anaemia
- decline in hearing
Rarely, severe hypothyroidism can cause myxedema coma, a life-threatening illness that needs immediate medical attention. Although the condition does not truly cause a coma, you could encounter:
- fatigue
- hypothermia
- reduced blood pressure
- minimal heartbeat
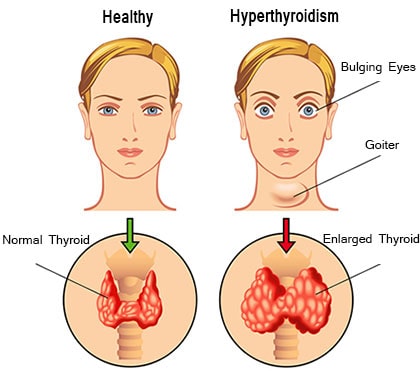
Causes of Hyperthyroidism
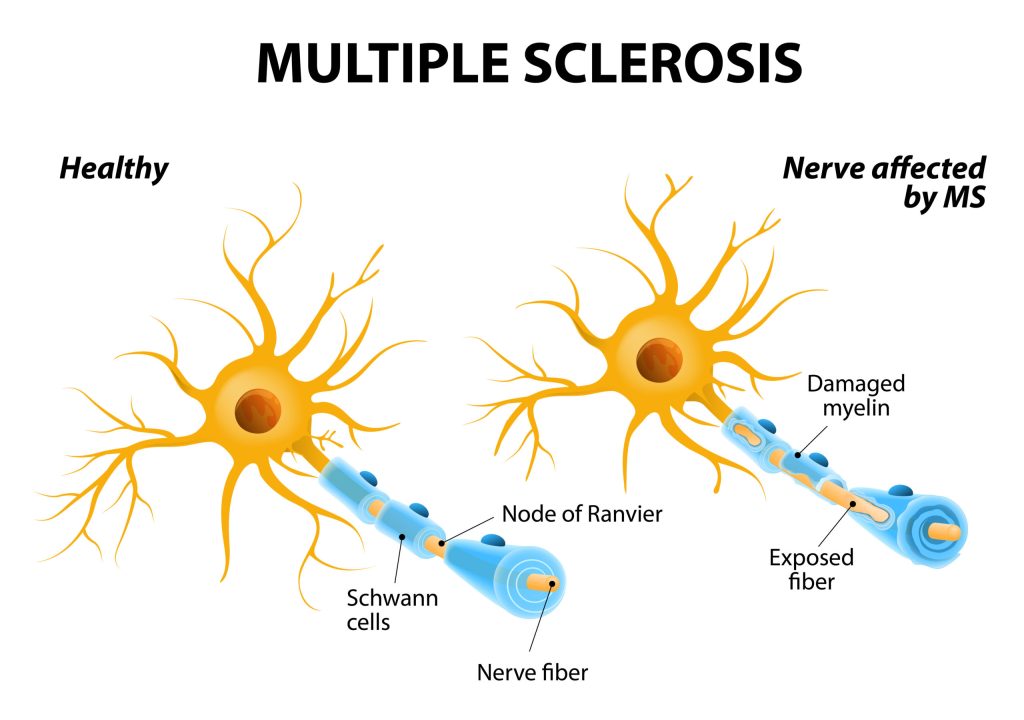
Both main and secondary causes can contribute to hypothyroidism. A disorder that directly affects the thyroid and makes it produce insufficient amounts of thyroid hormones is a key reason.
The pituitary gland’s malfunction, which prevents it from sending thyroid stimulating hormone (TSH) to the thyroid to regulate thyroid hormones, is a secondary reason.
There are a lot more prevalent primary causes of hypothyroidism. The most typical of these root causes is Hashimoto’s disease, an autoimmune disorder. This inherited illness is also known as chronic lymphocytic thyroiditis or Hashimoto’s thyroiditis (passed down through a family).
The thyroid is attacked and harmed by the body’s immune system in Hashimoto’s disease. As a result, the thyroid is unable to produce and release adequate thyroid hormone.
The following are some of the other main causes of hypothyroidism:
- Thyroiditis (inflammation of the thyroid).
- hyperthyroidism treatment (radiation and surgical removal of the thyroid).
- Iodine insufficiency refers to a lack of iodine in the body, which your thyroid needs to produce hormones.
- Hereditary disorders (a medical condition passed down through your family).
- Thyroiditis occasionally develops during a pregnancy (postpartum thyroiditis) or a viral disease.
Risk factors of hypothyroidism
The following elements can raise your risk of having hypothyroidism:
- being a woman
- 60 years of age or older
- receiving radiation therapy for your chest or neck
- being recently pregnant
- having thyroid issues run in one’s family
- possessing autoimmune disorders like Sjögren’s illness and type 1 diabetes
What happens if hypothyroidism is not treated?
If you do not receive treatment from a healthcare professional, hypothyroidism can develop into a serious and life-threatening medical disease. Your symptoms could worsen if you receive no treatment and could include:
- Developing mental health issues.
- having difficulty breathing
- being unable to keep a healthy body temperature.
- having cardiac issues
- acquiring a goitre (enlargement of the thyroid gland).
Myxedema coma, a dangerous medical condition, is another possibility. When hypothyroidism is not treated, this may occur.
REFERENCES:
- https://www.healthline.com/health/hypothyroidism/symptoms-treatments-more
- https://www.mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284
- https://my.clevelandclinic.org/health/diseases/12120-hypothyroidism
- https://www.webmd.com/women/hypothyroidism-underactive-thyroid-symptoms-causes-treatments
- https://www.endocrineweb.com/conditions/hypothyroidism
For more details, kindly visit below.