New guide on causes & prevention of cold and cough.
Tussis, commonly known as a cough, is a quick expulsion of air from the lungs and is a voluntary or involuntary act that clears the throat and breathing passage of foreign particles, bacteria, irritants, fluids, and mucus.
Coughing can occur unintentionally or as a reflex. Although coughing may indicate a dangerous illness, it usually goes away on its own without the need for treatment.
What is Common cold?
A viral infection that affects the upper respiratory tract is the common cold. The most frequent cause is a rhinovirus, and the most prevalent symptoms are a scratchy, sore throat, a stuffy or runny nose, and sneezing.

Sneezing, a stuffy or runny nose, and an itchy, sore throat are the typical early symptoms of the common cold. Because the common cold is so widespread, the majority of people can identify these early signs promptly. Adults actually have 2 to 3 colds on average each year.
The typical cold is basically an upper respiratory tract viral infection. More than 200 viruses have been found to cause colds. Rhinoviruses are the most widespread.
These viruses can quickly move from one person to another or from one surface to another. Many of these viruses can survive for hours or even days on surfaces.
While the common cold may be well known, there are some things you should know about this illness that can improve your health, help you avoid getting colds again, or even stop the virus from spreading to other people.
Symptoms of a cold
It normally takes 1 to 3 days for cold symptoms to manifest after being exposed to a virus that causes them. Rarely do cold symptoms arise suddenly.
Among the nasal symptoms are:
- congestion
- sinus tension
- clogged nose
- blocked nose
- loss of flavour or scent
- sneezing
- nasal fluid discharges
- discharge from the nose or throat postnasally
Head symptoms include:
- dripping eyes
- headache
- unwell throat
- cough
- an enlarged lymph node
Body-wide signs include:
- overall weariness or drowsiness
- chills
- bodily pains
- lower than 102°F (38.9°C) mild grade fever
- pain in the chest
- having trouble breathing deeply
A cold’s symptoms often last 7 to 10 days. On average, symptoms peak around day 5 and then gradually go better. However, you might have another disease, and it might be time to contact a doctor, if your symptoms intensify after a week or don’t go away after roughly 10 days.
Difference between a cold and flu
Since many of the symptoms of the two illnesses are similar, it can be challenging to distinguish between them. Both commonly occur in the colder months and have an impact on the upper respiratory system (nose, throat and trachea). But distinct viruses are responsible for colds and flu. The influenza virus is the source of the flu, but other other viruses are responsible for colds.
The key distinction between the flu and a cold is that the latter is more likely to cause fever and chills. Children can have fever with a typical cold, but adults seldom do.
In addition to physical aches, the flu has more severe symptoms than a cold. Issues from the flu can be fatal, but cold complications can also occur.
Diagnosing a cold
Most uncomplicated colds can be diagnosed without a trip to the doctor’s office. Frequently, all you need to know to make the diagnosis of a cold is its symptoms.
Make an appointment with a doctor if your symptoms persist for more than 10 days or get worse. Your doctor will be able to determine whether you are experiencing a separate health issue. If you have a cold, you can anticipate that the virus will leave your body in 7 to 10 days.
Until the virus has had a chance to run its course, you’ll probably only need to treat your symptoms if your doctor diagnoses a cold. These remedies can include of taking over-the-counter (OTC) cold remedies, drinking plenty of fluids, and getting lots of rest.
If you have the flu, it can take the same amount of time as a cold for the virus to completely go away. But it’s a good idea to follow up with your doctor if you discover your symptoms are growing worse after day 5 or if you don’t start feeling better after a week, as you might have developed another ailment.
If you have the flu, using an antiviral flu medicine at the beginning of the virus cycle may help. For those who have the flu, rest and hydration are also highly recommended. The flu simply needs time to circulate through your body, similar to how the common cold does.
Treatment of Cold
For adults
An upper respiratory tract viral infection causes the common cold. Antibiotics cannot be used to treat viruses. Most of the time, viruses like the common cold just require time to pass. Although the infection itself cannot be treated, the symptoms of the infection can be managed.
Over-the-counter (OTC) medications
The most widely used over-the-counter remedies for colds include:
- Decongestants. Drugs that decongest help relieve stuffiness and nasal congestion.
- Antihistamines. Antihistamines lessen the symptoms of a runny nose and help avoid sneezing.
- Pain reliever. Body aches, inflammation, and fever symptoms can be relieved with nonsteroidal anti-inflammatory medicines (NSAIDs), including ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin.
Combinations of these drugs are occasionally used in common cold treatments. If you use one, make sure to read the label and comprehend what you are taking so you don’t unintentionally take more of any one class of medication than you should.
The most typical negative effects of over-the-counter cold remedies include:
- dizziness
- dehydration
- mouth ache
- drowsiness
- nausea
- headache
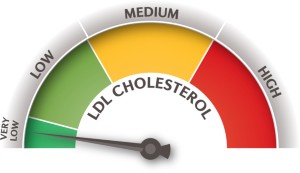
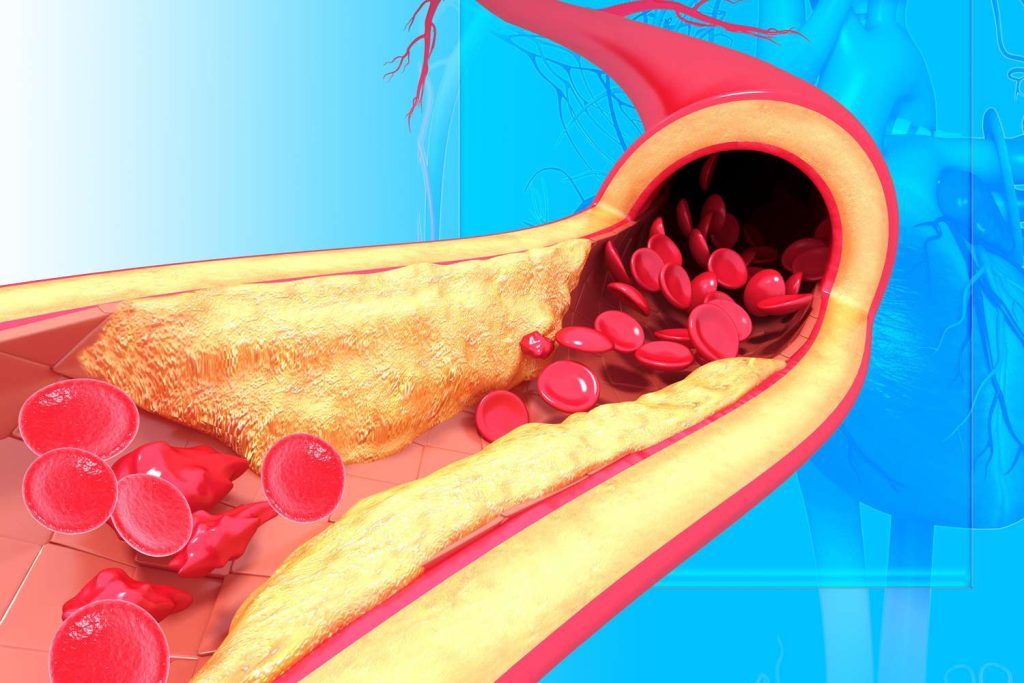
Prior to using any over-the-counter cold remedies, you should speak to your doctor if you’ve already been diagnosed with high blood pressure.
By constricting blood arteries and decreasing blood flow, several drugs assist treat symptoms. High blood pressure may impair the flow of blood throughout your body.
For Chidlren
The Food and Drug Administration (FDA) does not suggest over-the-counter (OTC) drugs for cough and cold symptoms in children under the age of two due to the possibility of significant and even fatal adverse effects.
With the aid of these natural treatments, you might be able to lessen a child’s cold symptoms:
- Rest. Children who are sick with a cold could be more worn out and agitated than usual. Allowing them to miss school would allow them to rest and recover from their cold.
- Hydration. It’s crucial that kids with colds drink enough of fluids. Colds can quickly make them dehydrated. Check to see whether they are drinking frequently. Wonderful water. Warm beverages, such as tea, can also ease a sore throat.
- Food. Attempt to find strategies to provide calories and fluids to children who may not feel as hungry as usual due to a cold. Soups and smoothies are both healthy choices.
- Gargle with salt water. Although gargling with warm, salty water isn’t the most enjoyable sensation, it can relieve sore throats. Nasal saline sprays can also assist in reducing nasal congestion.
- Warm baths. Mild aches and pains that are typical of colds may be reduced with a warm bath.
- A humidifier with cool mist. Nasal congestion can be reduced with the aid of a cool mist humidifier. Use of a warm mist humidifier should be avoided since it may enlarge the nasal airways and make breathing more challenging.
- Syringe for bulbs. Using a bulb syringe to suction the baby’s nasal passages is effective. Bulb syringes are often rejected by older kids.
REFERENCES:
- https://www.healthline.com/health/cold-flu/cold
- https://www.medicalnewstoday.com/articles/220349
- https://www.mayoclinic.org/diseases-conditions/common-cold/symptoms-causes/syc-20351605
- https://www.webmd.com/cold-and-flu/cold-guide/common_-cold-symptoms
- https://my.clevelandclinic.org/health/diseases/12342-common-cold
For more details, kindly visit below.