General causes, symptoms, & remedies to treat hemorrhoids.
Hemorrhoids develop when the veins around your anus swell, frequently as a result of constipation or straining during bowel movements. Hemorrhoids of a particular variety can be quite painful.
What is Hemorrhoids?
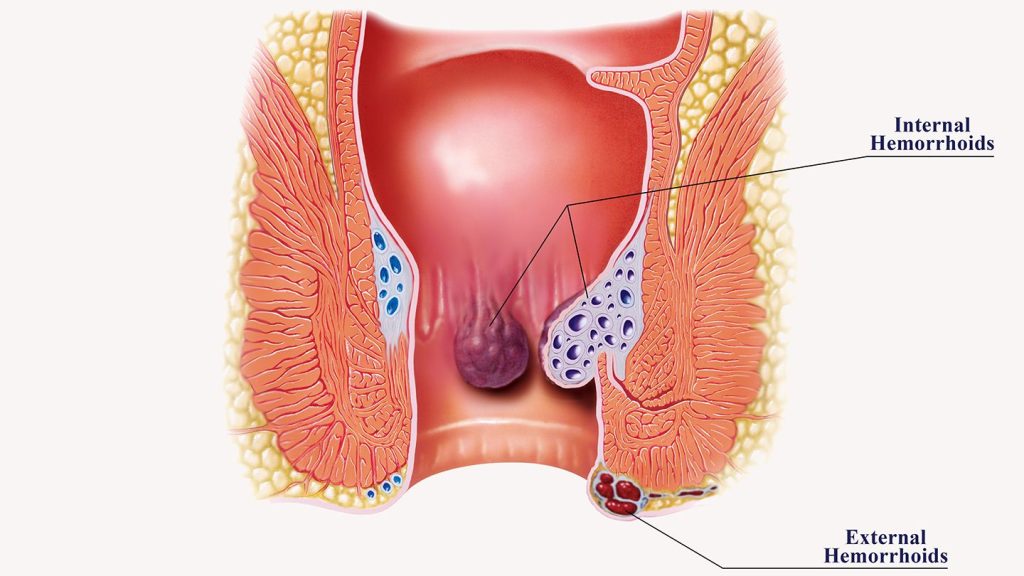
Hemorrhoids, often known as piles, are enlarged veins in the lower rectum and anus that resemble varicose veins. Internal haemorrhoids, which appear under the skin around the anus, are haemorrhoids that form inside the rectum (external hemorrhoids).
Nearly three out of every four adults will get haemorrhoids occasionally. There are numerous causes of haemorrhoids, however frequently the cause is not known. Fortunately, there are treatments for haemorrhoids that work. Home remedies and alterations in lifestyle help a lot of people.
Types of hemorrhoids
Your rectum may develop haemorrhoids inside or outside of it. Where the vein becomes enlarged determines the kind. Types consist of:
- Externally, the skin around your anus develops swollen veins. The canal in your anus is where your faeces exit. The irritation and pain of external haemorrhoids might vary. They bleed once in awhile. They sometimes become filled with blood that could clot. Although this is not harmful, it may cause pain and swelling.
- Internal: Your rectum develops swollen veins. The portion of your digestive system known as your rectum joins your colon (large intestine) to your anus. Although internal haemorrhoids might bleed, they often don’t hurt.
- Hemorrhoids can prolapse either internally or externally, which means they can stretch and enlarge outside of your anus. They could bleed or result in pain.
What causes hemorrhoids?
Hemorrhoids are a result of straining, which puts pressure on the veins in your rectum or anus. They may come to mind as varicose veins on your bottom.
Anal and rectal veins might swell and inflame as a result of any strain that puts more pressure on your tummy or lower extremities. The following factors might cause haemorrhoids to form:
- during a bowel movement, straining
- long periods of sitting, particularly on the toilet
- having persistent diarrhoea or constipation
- having haemorrhoids in your family
- carrying out regular heavy lifting or other physically demanding activities
- being overweight
- sexual activity that takes place anally, which might aggravate haemorrhoids
- having a baby (an enlarged uterus presses on the vein in the colon, causing it to bulge)
- being 50 years or older
Symptoms of hemorrhoids
The sort of haemorrhoids you have will determine your symptoms.
As a result of internal haemorrhoids,
- the presence of blood on tissue following a bowel movement
- skin that protrudes from the anus when a person urinates
Symptoms of an external haemorrhage include:
- intense itchiness in the anus
- unpleasant lump(s) or swelling(s) close to your anus
- Anus aches or pains, especially when sitting
Often, haemorrhoids don’t hurt. However, external haemorrhoids can occasionally cause a blood clot to grow on the skin. A thrombosed haemorrhoid is what this condition is. Hemorrhoids inside the body can also prolapse. Therefore, they won’t close themselves off inside the anus. Hemorrhoids that have prolapsed or that have thrombosed can be quite painful.
Hemorrhoids are not life threatening and frequently go away on their own without treatment, despite the fact that they can be very unpleasant.
Whenever you experience bleeding or black stools, see your doctor. Bleeding must be examined because it can have causes other than haemorrhoids. If after a week of home treatment, haemorrhoids don’t improve, consult a doctor as well.
How are hemorrhoids diagnosed?
The diagnosis of haemorrhoids may be made simply by looking at your anus. Your doctor might perform a separate examination to look for any anomalies inside the anus in order to confirm the diagnosis.
Known as a digital rectal exam, this test is performed. Your doctor will probe your rectum with a finger that is gloved and lubricated during this examination. Your doctor may prescribe an extra test such an anoscopy, sigmoidoscopy, or colonoscopy depending on your risk factors for digestive disorders.
Each of these examinations entails your doctor using a tiny camera to look for any irregularities in your colon, rectum, or anus. The interior of your anus is inspected by an anoscopy, the final two feet (50 centimetres) of your colon are investigated by a sigmoidoscopy, and the entire colon is investigated by a colonoscopy.
In these exams, a tiny fiber-optic camera is introduced into a tiny tube that is placed in your rectum. Your doctor may inspect the haemorrhoid up close with the help of this test since it provides a clear picture of the interior of your rectum.
Treatment options for hemorrhoids
Hemorrhoids can be treated at a doctor’s office or at home.
Pain reduction
Spend at least 10 minutes each day in a warm tub of water to reduce pain. To ease the discomfort of external haemorrhoids, you can also sit on a warm water bottle.
Use an over-the-counter (OTC) medication suppository, ointment, or cream to ease the burning and itching if the pain is intolerable. Hemorrhoid suppositories are available both online and offline.
Fiber-rich foods and supplements
You can also use an over-the-counter fibre supplement if you have constipation to assist soften your stools. The supplements psyllium and methylcellulose are two examples of this kind.
A home remedy
Your discomfort from haemorrhoids can be reduced by over-the-counter topical medications like hydrocortisone or haemorrhoid cream. Witch hazel pads can also provide relief from haemorrhoids.
- Both hydrocortisone and haemorrhoid cream are available online.
- It may also be beneficial to soak your anus for 10 to 15 minutes each day in a sitz bath.
- Every day, take a shower or bath and wash your anus with warm water to maintain proper cleanliness. However, avoid using soap because it can make haemorrhoids worse. Additionally, when wiping after a bowel movement, avoid using toilet paper that is dry or scratchy.
- Your anus can benefit from applying a cold compress to lessen haemorrhoid swelling. Acetaminophen, ibuprofen, or aspirin are examples of painkillers that can help with discomfort or pain.
Medical procedures
Your doctor might advise obtaining a rubber band ligation if self-care measures are unsuccessful in treating your haemorrhoids. During this operation, the doctor ties a rubber band around the haemorrhoid to stop blood flow to it.
As a result, the haemorrhoid loses circulation and must contract. A medical practitioner should be the only one to carry out this surgery. Don’t attempt this alone.
Injection treatment, also known as sclerotherapy, may be used by your doctor if rubber band ligation is not a possibility for you. Your doctor directly injects a drug into the blood vessel during this treatment. The haemorrhoid becomes smaller as a result.
Prevention of hemorrhoids
Steer clear of straining when having a bowel movement to stop or stop haemorrhoids from getting worse. Try to consume more water as well. Getting adequate water can prevent the hardness of your faeces.
To stop haemorrhoids from forming, use the bathroom as soon as you begin to feel a bowel movement coming on. Avoid sitting for extended periods of time, especially on hard surfaces like concrete or tile, to prevent constipation. Exercise frequently.
The likelihood of having haemorrhoids later on can be reduced by eating meals high in dietary fibre. Good sources of dietary fibre include:
- whole grain
- brow risotto
- oatmeal
- pears
- carrots
- buckwheat
- bran
Dietary fibre aids in the development of intestinal bulk, which softens the stool and makes it simpler to pass.
REFERENCES:
- https://www.healthline.com/health/hemorrhoids
- https://www.medicalnewstoday.com/articles/73938
- https://www.mayoclinic.org/diseases-conditions/hemorrhoids/symptoms-causes/syc-20360268
- https://my.clevelandclinic.org/health/diseases/15120-hemorrhoids
- https://www.webmd.com/digestive-disorders/understanding-hemorrhoids-basics
For more details, kindly visit below.