Explore each types of Colitis and its numerous symptoms.
When your big intestine becomes inflamed, colitis develops. It can result in discomfort as well as other symptoms like ulcers, bloating, and diarrhoea. Different therapies are needed for various forms of colitis.

Your colon, sometimes referred to as your large intestine, is inflamed when you have colitis. You will have abdominal discomfort and agony if you have colitis. This discomfort could be modest and recurrent over time, or severe and striking out of nowhere.
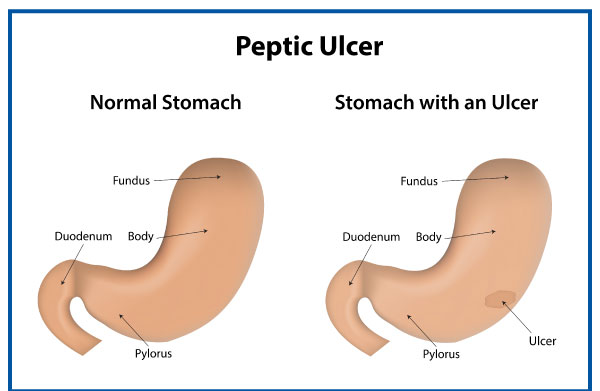
On the colon’s lining, ulcers can develop in serious situations. These ulcers may bleed, resulting in the production of pus and mucous. There are many different drug options, and doctors can customise the course of treatment to match specific needs.
Types and causes of colitis
Ulcerative colitis
One of two disorders categorised as inflammatory bowel disease is ulcerative colitis (UC). The second is Crohn’s illness. The inner lining of your large intestine becomes inflamed and develops bleeding ulcers as a result of the chronic condition known as UC. Typically, it starts in the rectum and progresses to the colon.
The most typical colitis diagnosis is UC. Experts don’t know why the immune system overreacts to bacteria and other chemicals in the digestive tract, which causes it to happen.
Typical forms of UC include:
- Proctosigmoiditis, a condition that affects the rectum and lower colon,
- Left-sided ulcerative colitis, which starts from the rectum and affects the left side of the colon.
- Having an effect on the entire large intestine, pancolitis
Pseudomembranous colitis
The expansion of the bacterium Clostridium difficile causes pseudomembranous colitis (PC) (C. diff). In the intestine, this type of bacteria is typically present, but because “good” bacteria exist to balance it out, it doesn’t create any issues.
Antibiotics in particular are known to kill beneficial bacteria. This enables C. diff to take control and release inflammatory toxin-producing toxins.
Ischemic colitis
When blood supply to the colon is abruptly cut off or reduced, ischemic colitis (IC) develops. A abrupt blockage may be brought on by blood clots. The most common cause of recurrent IC is atherosclerosis, or the accumulation of fatty deposits in the blood arteries supplying the colon.
This kind of colitis frequently results from underlying diseases. These may consist of:
- An inflammatory condition of the blood vessels is called vasculitis.
- diabetes
- stomach cancer
- dehydration
- losing blood
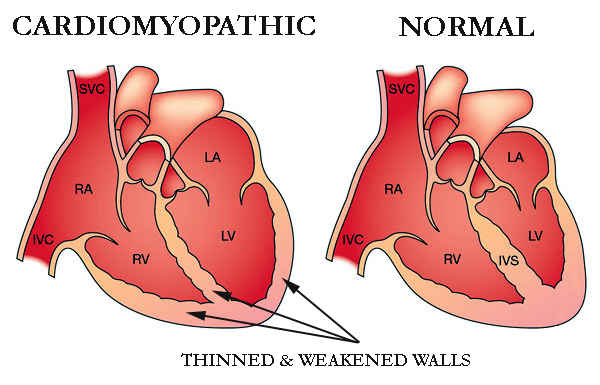
- heart disease
- Blockage or hindrance
- injury or trauma
Although it’s uncommon, taking certain medications, including fibrates and nonsteroidal anti-inflammatory drugs, can cause IC (NSAIDs). To fully comprehend all drugs that might be a contributing component, more research is required.
Microscopic colitis
A physician can only diagnose microscopic colitis by using a microscope to examine a sample of colonic tissue. A doctor will search for inflammation-related indicators, such as white blood cells called lymphocytes.
Occasionally, doctors would divide microscopic colitis into lymphocytic and collagenous colitis. When a large number of lymphocytes are found, a doctor says the patient has lymphhocytic colitis. The tissues and lining of the colon, however, are not abnormally thickened.
Collagenous colitis is a condition in which the outermost layer of tissue of the colon’s lining thickens abnormally as a result of an accumulation of collagen. Doctors are unsure of the specific cause of microscopic colitis. They are aware that certain persons are more susceptible to the disease than others.
People who are more vulnerable are:
- habitual smokers
- individuals who were born as females
- persons who have had an autoimmune disease in the past
- those over the age of 50
- those who take specific medications, such as some varieties of:
- proton pump blockers (PPIs)
- inhibitors of selective serotonin reuptake (SSRIs)
- Aspirin and other NSAIDs (nonsteroidal anti-inflammatory medications)
The following are the signs and symptoms of microscopic colitis:
- persistent diarrhoea
- stomach bloating
- abdominal pain
Babies with allergic colitis
Infants are susceptible to the disorder known as allergic colitis, which typically appears in the first few months following birth. Infants with the syndrome may have the following symptoms:
- reflux
- uncontrollable spitting up
- fussiness
- potential blood specks in a baby’s poop
Doctors are unsure of the specific cause of allergic colitis. One of the most widely accepted explanations is that some components in breast milk cause allergic or hypersensitive reactions in newborns with allergic colitis. A review of papers published in 2020 suggested that formula, cow’s milk, or breast milk protein allergies may be at blame.
Infants with similar symptoms may also develop an allergic colitis called eosinophilic colitis. Similar to that, its causes are unknown, but they are probably connected to a protein allergy.
Symptoms of Colitis
Typically, diarrhoea is ulcerative colitis’s initial sign. Stools becoming gradually looser, and some people may get cramping in their stomachs and have a strong urge to use the restroom.
The onset of diarrhoea may be gradual or abrupt. The degree and spread of inflammation affects the symptoms.
The following list of ulcerative colitis symptoms is common:
- abdomen ache
- crimson and mucus-filled diarrhoea
Some folks might also go through:
- drowsiness or tiredness
- slim down
- reduced appetite
- anaemia
- an increased temperature
- dehydration
- a persistent urge to urinate
Early in the morning is usually when symptoms are worse. Mild or nonexistent symptoms may last for months or years at a time. However, depending on the area of the colon that is afflicted, they frequently come back without therapy.
Risk factors of colitis
Following are a few well-known risk factors for ulcerative colitis:
- Age: Although ulcerative colitis can affect anybody, it is more prevalent in people between the ages of 15 and 30.
- Ethnicity: White people and persons of Ashkenazi Jewish origin are more likely to develop the illness than other ethnic groups.
- Genetics: Although new research has discovered particular genes that may contribute to ulcerative colitis, the relationship is unclear because environmental variables also play a part.
Diagnosis of Colitis
Your symptoms may be frequently asked about by your doctor, along with when they first appeared. The doctor will do a complete physical examination and use diagnostic procedures like:
- A flexible tube with a camera is inserted through the anus to see the rectum and colon during a colonoscopy.
- Similar to a colonoscopy but only displaying the rectum and lower colon, sigmoidoscopy
- stool specimens
- scans of the abdomen using MRI or CT technology
- ultrasonography, which, depending on the area being examined, can be useful
- An X-ray of the colon taken after it has been injected with barium, which improves image clarity, is known as a barium enema.
Treatment of colitis
Treatments, which attempt to lessen symptoms, can differ depending on things like:
- a kind of colitis
- age
- overall state of health
Bowel rest
Limiting your oral intake can be beneficial, especially if you have IC. It could be required to administer fluids and other nutrients intravenously at this time.
Medication
To help you control the symptoms of colitis, your doctor may recommend a number of drugs. These medicines may consist of:
- Corticosteroids or 5-aminosalicylates are examples of anti-inflammatory drugs that can be used to alleviate pain and swelling.
- immune system suppressants such cyclosporine, azathioprine, or tofacitinib (Xeljanz) (Gengraf, Neoral, Sandimmune)
- Biologics like ustekinumab, adalimumab, and infliximab (Remicade) (Stelara)
- antibiotics for infection treatment
- taking painkillers
- antibiotics for diarrhoea
- spasmolytic medications
- nutritional deficiency supplements
Surgery
Your colon or rectum may be completely or partially removed during surgery for colitis. In the event that other therapies fail, this might be required.
Prevention of colitis
Surgery is the only surefire method of avoiding a flare-up of colitis. You can lessen the likelihood of flare-ups by doing the following if you want to avoid surgery:
- To keep note of the things that can make symptoms worse, keep a food journal.
- Find out from your doctor whether you should alter how much fibre you consume.
- Ask your doctor if eating more frequent, smaller meals will benefit you.
If you can, up your level of activity. - Learn stress-reduction techniques like yoga, meditation, and mindfulness practises.
- Always follow the directions on your prescriptions, and let your doctor know if you haven’t.
- Make sure your doctor is aware of all of your other prescription and over-the-counter medications, as well as vitamins.
REFERENCES:
- https://www.healthline.com/health/colitis
- https://www.medicalnewstoday.com/articles/163772
- https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis
- https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326
- https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/what-is-ulcerative-colitis
For more details, kindly visit below