Analyze the links between BMI, obesity & cognitive ability.
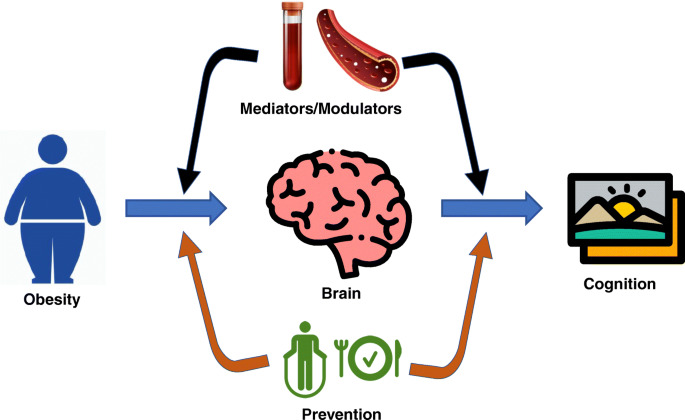
According to the World Health Organisation (WHO), there were more than 650 million obese adults in the world as of 2016. Obesity has been linked in the past to an increased risk of cognitive deterioration.
Evidence from University College London researchers challenges the idea that fat and cognitive capacity are causally related.
Around the world, more than 1.9 billion adults were obese in 2016, with more than 650 million of those adults suffering from obesity, a disease in which a person’s weight is over normal ranges and may lead to various health issues.
According to current estimates, 167 million adults and children will be overweight or obese by 2025. A multitude of disorders, including diabetes, cardiovascular disease, hypertension, osteoporosis, rheumatoid arthritis, and cancer, have been linked to obesity in previous studies, including these.
Furthermore, previous research has connected obesity to a higher risk of cognitive deterioration.
The causal relationship between obesity and cognitive performance has now been called into question by University College London academics. They contend that common family variables have tainted the research linking cognitive aptitude and BMI.
Obesity
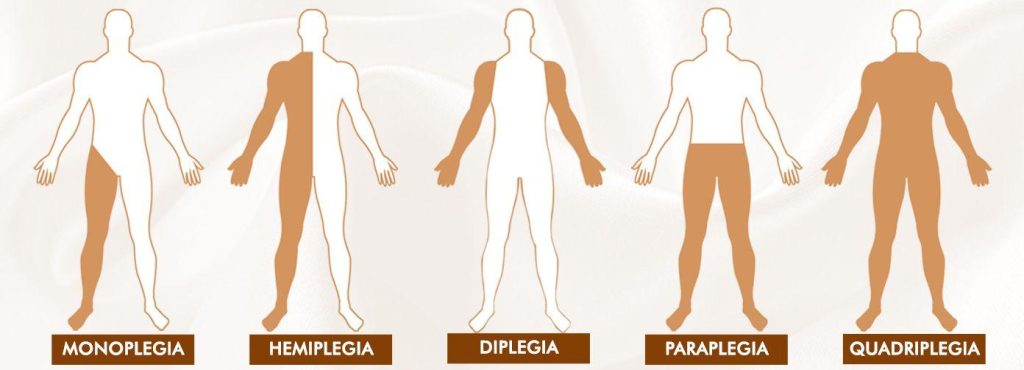
If a person’s present weight is excessive for their height, they are considered obese. The body mass index (BMI) is the most popular metric for determining a person’s level of obesity.
This tool determines if an adult is obese or not based on their height and current weight:
- BMI less than 18.5 indicates underweight.
- Suitable BMI range: 18.5-24.9
- BMI of 25 to 29.9 indicates obesity
- obesity: a BMI of 30 or above
Children and teenagers need a different BMI calculator, which considers height, age, and gender to evaluate obesity because they are still developing.
The BMI measurement is not without problems, though. It is unable to distinguish between muscle and fat when weighing someone. Additionally, it disregards a person’s race, overall body composition, or bone density.
Cognitive function and obesity
Lead author of this study and senior research fellow at the Centre for Longitudinal Studies at University College London in the U.K., Dr. Liam Wright, Ph.D., states that there are several reasons why the research team decided to investigate the causal relationship between cognitive capacity and obesity:
“Over the past forty years, there has been a significant rise in the prevalence of obesity, but BMI hasn’t increased uniformly throughout the population. Therefore, it is crucial to understand why some people are more predisposed to obesity than others.
Additionally, there is a substantial body of research in the field of cognitive epidemiology that demonstrates a connection between cognitive function and practically every measure of health and health behaviour, including obesity.
Unfortunately, the majority of the cognitive epidemiology literature employs observational research designs that may be biassed and fail to show causal effects, according to Dr. Wright. “There are some compelling theoretical arguments for why cognitive ability might have a causal effect on health, but regrettably, these arguments are based on observational research designs,” she said. Because a sibling design could take into account some of the variables that can skew relationships found in previous research, we felt it was crucial to investigate for a relationship between cognitive capacity and BMI.
Examining siblings to reduce bias
Dr. Wright and his research group evaluated data from four distinct young population cohort studies carried out in the United States that included 12,250 siblings from 5,602 homes. Each participant’s data were tracked from youth to age 62.
The scientists were able to take into consideration unobserved characteristics associated with family background by analysing the relationship between cognitive capacity and BMI among families.
“Sibling designs account for factors that are shared between siblings by design,” Dr. Wright said. They don’t require the measurement of these factors, which is both a benefit and a drawback because it is difficult to determine which common factors actually contribute.
With this qualification, he continued, “There are four main factors that we thought might be significant: genetics (siblings share 50% of DNA), parental socioeconomic class (wealth, location, etc.), parenting styles (particularly regarding dietary choices), and parental cognitive ability (cognitive ability could operate indirectly!). “Once more, we didn’t directly examine these.”
According to Dr. Wright, they predicted that these variables would make general population studies more biassed and lead to weaker relationships than in earlier studies, which is exactly what they found.
However, he cautioned, “remember that sibling designs have their own flaws, including the ability for siblings to influence one another, for example, by modelling one another’s behaviour. This may imply that our findings are also skewed, albeit downwardly and smaller than the actual causal effect.
Association between BMI and cognitive ability
When the researchers evaluated the data from study participants who were not related, they discovered that, after accounting for family socioeconomic status, the change in teenage cognitive capacity from the 25th to the 75th percentile was associated with an estimated 0.61 kg/m drop in BMI.
And when the researchers analyzed the information from siblings, they discovered that the change in BMI from the 25th to the 75th percentile of teenage cognitive ability was only correlated with a 0.06 kg/m drop in cognitive capacity.
The relationship between cognitive capacity and BMI was less pronounced when siblings were compared than when the entire population was, according to Dr. Wright, but he was not surprised by this given the overall characteristics he mentioned.
However, he noted, “I was shocked at how little of an association there was when comparing siblings. As said, there are strong arguments to support the idea that cognitive ability has an impact on health and health-related decision-making“.
“Two possibilities for this small association are that one, our results were biassed towards finding smaller associations (e.g., by siblings influencing each other), and two, reflective decision-making isn’t as important in determining BMI as other factors like satiety, etc.,” Dr. Wright continued. Both of these are hypothetical.
Unproven causality
As a parent and a neurologist, Dr. Segil claimed that he has never observed a connection between obesity or a healthy weight and cognitive aptitude in people.obese
The purpose of this study, according to Dr. Segil, “is to argue that people with higher cognitive abilities, who have a higher socioeconomic position, have made healthier decisions.” Additionally, it’s possible that people’s cognitive function increases as their BMI decreases when they make healthier decisions.
He continued, “I do not believe that there is any evidence linking obesity to cognitive function. And I believe that their research’s use of siblings or other family members who are in a similar social economic situation to real-life situations such as brothers or sisters or siblings is realistic.”
After reading this study, Dr. Segil stated that he would be curious to know whether maternal or paternal obesity had a greater impact on adolescent cognitive development.
As a result of reading this, they claimed that adolescent cognition is linked to a lower adult BMI, he continued. So I’m keen to know if stronger adolescent cognitive abilities are related to the maternal and paternal BMI. Does having a thin or fat parent, using the same dataset, alter their children’s cognitive ability?I was shocked, though, by how little of an association there was when comparing siblings. As mentioned, there are strong arguments to support the idea that cognitive ability has an impact on one’s health and decision-making in relation to their health.
RFERENCES:
- https://www.medicalnewstoday.com/articles/bmi-obesity-and-cognitive-ability-sibling-study-questions-link
- https://eurapa.biomedcentral.com/articles/10.1186/s11556-022-00284-2
- https://www.frontiersin.org/articles/10.3389/fendo.2022.953826/full
For Cognitive disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_478