Reduce the Dementia risk by strict blood pressure control.
The effects of intensive versus routine hypertension treatment on brain lesions were examined by researchers at the University of Texas Health Science Centre in San Antonio.
The researchers discovered that intensive therapy that maintains blood pressure within normal bounds is associated with a slowed progression of lesions using data from a previous study.

The study results could influence treatment strategies for hypertensive patients to lower the likelihood of lesions that can result in diminished cognitive performance with further research and trials.
Millions of people have hypertension, which can lead to strokes and brain lesions and compromise brain health.
An aggressive blood pressure regimen can slow the growth of white matter lesions in the brain, according to a recent study headed by UT Health San Antonio.
In contrast to patients with systolic blood pressure readings of 140 mm Hg, the researchers compared the MRI scans of individuals who maintained blood pressure levels below 120 mm Hg.
What is considered hypertension?
Millions of Americans suffer from the medical disease known as hypertension, sometimes known as high blood pressure. Nearly half of American adults have hypertension, which the Centres for Disease Control and Prevention claim contributed to more than 670,000 deaths in 2020.
Blood vessel damage and other health issues can result from high blood pressure. Heart attacks and strokes are two conditions brought on by hypertension.
The following blood pressure ranges are described by the American Heart Association:
For individuals, a normal blood pressure reading is defined as an upper number (systolic) less than 120 over a lower number (diastolic) of 80 mm Hg.
- Blood pressure that is elevated is 120 to 129 over 80 or less.
- Hypertension in stage 1 is defined as 130-139 above 80-89.
- 140 over 90 or higher indicates stage 2 hypertension.
When the systolic and/or diastolic values exceed 180 and 120 respectively, a hypertension crisis ensues.
As the cardiologist, Dr. Kershaw Patel points out in the Houston Methodist podcast On Health, “When we talk about high blood pressure, we must realise it affects not just the heart, but also the brain, the kidneys, and other organs in the body.”
Although doctors frequently prescribe prescription drugs to treat high blood pressure, patients can also try to lower or normalise their blood pressure by making changes to their lifestyle.
Dr. Patel stated that lifestyle changes and then drugs are commonly used to manage high blood pressure. And it really comes down to two-thirds lifestyle and one-third medicine. By adjusting a few aspects of our lifestyle, we can significantly lower our blood pressure.
Blood pressure can be normalised by giving up smoking, consuming less alcohol, exercising, eating a low-sodium diet, and eating more fruits and vegetables.
lowering one’s blood pressure to 120
The American Academy of Family Physicians’ (AAFP) standard of care for hypertensive patients is to lower their systolic blood pressure to 140 mm Hg. This goal lowers the risk of cardiovascular death, according to the AAFP.
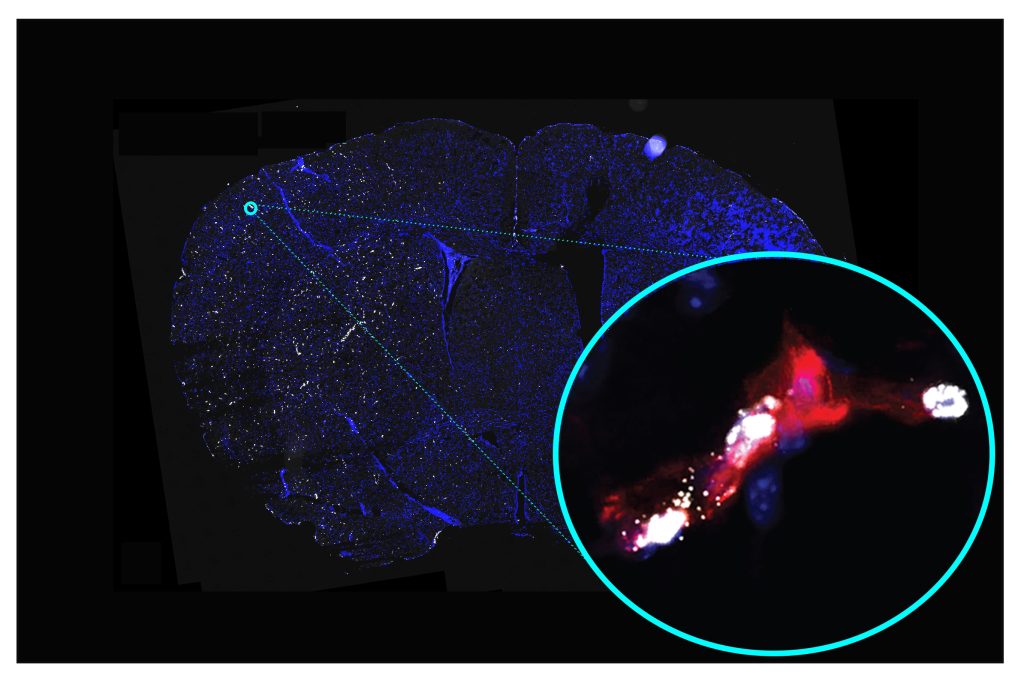
To assess the effect on white matter lesions (WMLs), the UT Health San Antonio researchers compared the normal treatment target to a more rigorous therapy. The goal of the rigorous treatment program was to lower participants’ systolic blood pressure to under 120 mm Hg.
The researchers examined data from 458 participants using information from the Systolic Blood Pressure Intervention Trial (SPRINT), which tracked participants for 4 years. Participants in the study were “aged 50 years or older with hypertension and without diabetes or a history of stroke,” according to the study’s authors.
At the start and conclusion of their trials, the researchers matched each participant’s treatment to their MRI images. They were searching for WMLs, a type of injury to the brain’s white matter that can result in cognitive impairment.
Treatment that is intensive lessens brain damage
According to the study’s findings, the intensive treatment group’s WML volume progression and fractional anisotropy (FA) declines were slower than those of the conventional treatment group.
The FA result is noteworthy since it represents a “measure of connectivity in the brain.” The right splenium, right tapetum, and left anterior corona radiata are a few of the brain areas that saw slower WML growth.
The study also demonstrates that aggressive blood pressure management may be able to maintain some myelin structure, which, according to the scientists, “ultimately slows the progression of injury patterns associated with dementia.”
According to research author Dr. Tanweer Rashid, who works with the Biggs Institute at UT Health San Antonio, “our study shows that specific areas have greater benefit, representing sensitive regions to track in future trials evaluating small-vessel disease.”
How white matter is impacted by blood pressure?
The study’s findings were discussed by Dr. Arun Manmadhan, a cardiovascular disease expert at Columbia University Irving Medical Centre in New York City.
“White matter lesions are abnormally damaged regions of tissue in the white matter of the brain. According to Dr. Manmadhan, they are frequently brought on by anomalies in the tiny blood arteries that provide oxygen and nutrients to the brain.”
Dr. Manmadhan provided more information on the study’s findings, namely how blood pressure may affect WMLs.
“The current report, which is a SPRINT-MIND substudy, examined the impact of stringent blood pressure management on changes in the brain’s white matter as determined by MRI.”
According to Dr. Manmadhan, the results here point to a potential benefit of tight blood pressure control in slowing the development and progression of white matter lesions, which are linked to a higher risk of dementia and cognitive decline.
Overall, according to Dr. Manmadhan, the study is an asset to the field of hypertension.
This study “adds to the already substantial body of literature that managing blood pressure is very important for not only preventing cardiovascular events but also in maintaining memory and cognition,” the author added.
REFERENCES:
- https://www.medicalnewstoday.com/articles/strict-blood-pressure-management-may-lower-dementia-risk
- https://www.heart.org/en/news/2023/01/23/intensive-blood-pressure-control-may-lower-risk-for-cognitive-problems-in-more-people
- https://www.health.harvard.edu/mind-and-mood/some-blood-pressure-drugs-may-lower-dementia-risk
For Dementia disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_478