Focused ultrasound can improve Parkinson’s symptoms?
In a recent study, a novel, non-invasive method of using focused ultrasound to lessen Parkinson’s disease symptoms was presented. In order to disrupt the neural network that causes uncontrolled movement and motor dysfunction, the approach entails deleting a tiny neuron cluster.
Twice as many research participants received the new treatment than those who received sham care, and these improvements in symptoms frequently sustained for at least a year.
An innovative, noninvasive strategy for lowering dyskinesia, or uncontrollable movements, and motor impairment in Parkinson’s disease patients is presented in a recent study. Focused ultrasound is used in the novel technique.
When compared to trial participants who underwent a sham, or placebo, therapy, twice as many people reported improvement in dyskinesia and motor impairment three months after undergoing the incision-less procedure.
In 77% of individuals who responded to the medication, the gains persisted for up to a year. Patients who receive focused ultrasound therapy often return home the same day.
Gait issues, speaking difficulty, and eye disruption were among the infrequently reported negative effects by the researchers. The group that received the treatment experienced more severe adverse effects than the group that received a placebo.
Focused ultrasound
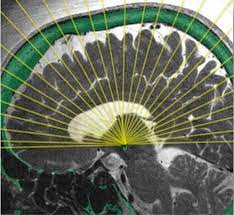
Focused ultrasound is a minimally invasive, non-surgical technique that causes an ablation in a region that reduces Parkinson’s and tremor symptoms. To produce a clear thermal lesion deep into the brain without harming nearby structures, we use focused ultrasonic waves. The basal ganglia are what we are primarily aiming for. A set of brain regions are involved in the coordination and control of movement. We employ a thermal imaging equipment for magnetic radiofrequency imaging (MRI) during the procedure. This gauges alterations in the skull’s temperature and enables us to guarantee the patient’s security.
The treatment is fantastic because it allows us to work on really delicate places securely, effectively, and with very minimal adverse effects.
Dopamine and L-DOPA
Parkinson’s disease is caused by low levels of the neurotransmitter dopamine in the substantia nigra of the brain. This is brought on by the death of neurons that produce dopamine.
The predominant idea holds that autophagy, the brain’s housekeeping mechanism, has failed, causing an accumulation of waste that impairs brain function.
Dopamine synchronises various brain regions so that they are communicating with one another at the same frequency, according to Dr. Jean-Philippe Langevin, director of the Pacific Neuroscience Institute’s Restorative Neurosurgery and Deep Brain Stimulation Program, who was not involved in the study.
“Consider all these parts of the brain as walkie-talkies or phones trying to communicate, but the frequency at which they’re trying to communicate is off,” said Dr. Langevin. Movements become stiff, hesitant, and tremble as a result, and are no longer flowing.
Dr. Langevin stated that the absence of dopamine causes the motor system of the brain, which regulates movement, to be “quite noisy.” Researchers can actually recognise electrical noise as this “noise.” According to recent research, Parkinson’s disease actually causes some neuronal frequencies to rise.
Levodopa, also known as L-DOPA, which replenishes dopamine in the brain, is the most widely used medication for the illness.
Yet, for many people, the dyskinesia and motor dysfunction they encounter are genuine side effects of L-DOPA therapy. Over time, the medication’s effectiveness deteriorates as well.
New treatment
The novel method examined in the trial is based on an essential tremor medication that was previously authorised in 2016.
A small group of neurons in the globus pallidus area of the brain are removed or ablate during focused ultrasound therapy. By leaving scarring on the tissue, ablation causes tissue destruction.
Dr. Howard M. Eisenberg, co-author of the study and professor of neurosurgery at the University of Maryland Medical System, with the following explanation of how a little more than 1,000 sound energy beams ablate the target tissue:
“Like light, sound can be concentrated. Imagine you had a magnifying glass when you were a child. If you focused the sun’s rays on a piece of paper, you would receive a tiny dot of light that would then transform into heat and burn a hole in the paper. With sound, we may achieve the same results.
When the beams are concentrated and the intensity is strong enough, “you can burn a little hole in the brain” precisely at the target location without harming surrounding tissue, he told us.
In essence, Dr. Eisenberg said, “that’s how it works: Back to the future, similar to ablation that was done years ago for essential tremor, but using different technology.”
According to Dr. Eisenberg, the dyskinesia and motor dysfunction are not always brought on by the ablated neurons. Instead, “it’s a system of targets that are interconnected nuclei, and you’re interrupting that system,” he said.
Motives for excitement
If the procedure enables Parkinson’s patients to take less L-DOPA medication, then there are many reasons to be optimistic, according to Dr. Langevin.
According to Dr. Eisenberg, based on prior experience with essential tremor ablation, we can anticipate benefits in roughly 80% of patients, and they might last at least five years.
However, not every participant in the research benefited from this treatment. A few participants, according to Dr. Eisenberg, might have skulls that are less effective at transmitting acoustic energy.
The reason for this is that the skull is made up of two hard layers of bone sandwiched by a softer layer, “like an Oreo biscuit,” rather than being one solid piece of bone.
Focused ultrasound vs. DBS
Dr. Eisenberg pointed out that deep brain stimulation is thought to be more successful for treating essential tremors than ablation (DBS). DBS stimulates tissue rather than destroying it. Furthermore, Parkinson’s dyskinesia and motor disability are treatable by DBS.
DBS, however, necessitates creating one or more tiny holes in the skull through which a wire is placed and directed to the desired location in the brain. The wire is then attached to a tiny neurostimulator that has been inserted into the chest.
“They won’t consider it even though we always explain that deep brain stimulation has advantages over focused ultrasound,” Dr. Eisenberg said of individuals who would prefer it instead. Hence, it’s beneficial for individuals who simply don’t want deep brain stimulation, which is understandable.
Yet, he added, the advantages provided by the new focused ultrasound approach are still potent enough to be life-altering.
REFERENCES:
- https://news.unchealthcare.org/2023/02/new-focused-ultrasound-effective-for-treating-parkinsons-movement-disorders/
- https://www.pennmedicine.org/updates/blogs/neuroscience-blog/2021/december/focused-ultrasound-and-parkinsons
- https://www.medpagetoday.com/neurology/parkinsonsdisease/103225
- https://www.medicalnewstoday.com/articles/medical-myths-all-about-parkinsons-disease
For more details, kindly visit below.