Explore the latest link between MS and Your Gut.
The central nervous system is impacted by the chronic disease known as multiple sclerosis (MS). When the immune system targets the outer layer of nerve cells, symptoms including weakness in the muscles and visual issues appear.
MS’s precise causation is unknown, however scientists believe that a number of variables may be involved. A recent study discovered that MS may be brought on in persons with a genetic predisposition by a toxin produced by a common gut bacterium.

Multiple sclerosis (MS) is a persistent nerve system disease. Young adults between the ages of 20 and 40 are the most frequently affected, and women are more likely than males to experience it.
There are around 2.8 million MS sufferers worldwide, and the number is growing, according to the Multiple Sclerosis International Federation (MSIF).
Symptoms of Multiple Sclerosis
The immune system of the affected person destroys the myelin sheath that protects the nerve fibers in this autoimmune illness. Sclerosis is a scar or lesion that results from damage. These lesions, which most frequently affect the central nervous system, can cause a variety of symptoms, such as:
- muscular tremor
- feeling numb and tingly
- bowel and bladder issues
- vision issues
- fatigue
- nausea and vertigo
- Painful muscular spasms.
Relapsing-remitting MS, the most prevalent type of MS that accounts for 85% of cases, is characterised by episodes of new or worsening symptoms and intervals during which symptoms subside or go away.
Scientists believe that environmental variables and genetic vulnerability may play a role in the development of the illness, while the specific reason is yet unknown. MS is riddled with many mysteries.
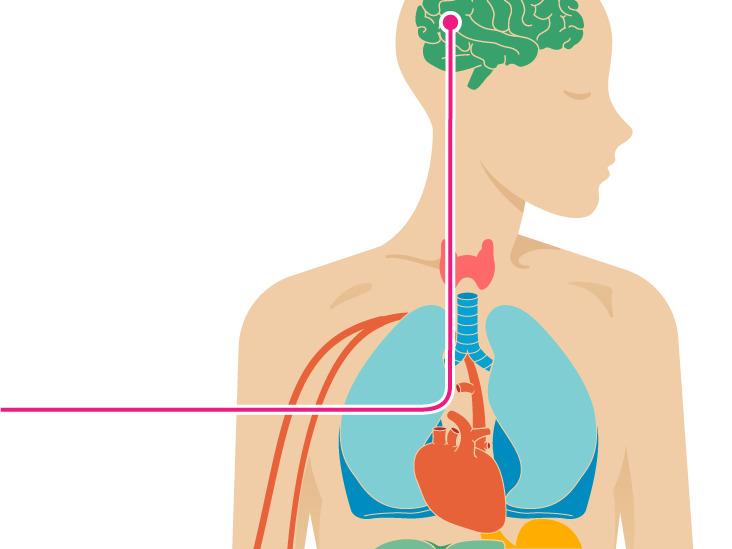
Epsilon toxin, which is produced by a bacteria that may be found in the small intestine, has now been linked to the development of MS and the maintenance of symptoms, according to study conducted by researchers at Weill Cornell Medicine’s Brain and Mind Research Center.
How the gut microbiota affects MS?
The trillions of bacteria that reside in your digestive system make up the gut microbiota. The majority of microbes are bacteria, but they can also include viruses, fungi, and the microscopic, single-celled creatures known as protozoa.
In general, these bacteria are beneficial and even essential to our health. Yet, dysbiosis, or an out-of-balance microbiota, can cause issues. According to studies, alterations in the microbiota may be a factor in various autoimmune diseases.
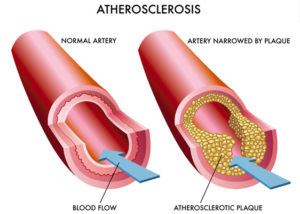
In MS patients, changes to the gut flora are frequent. According to this recent study, patients with MS are more likely than healthy controls to carry the pathogen Clostridium perfringens. Epsilon toxin, which is produced by C. perfringens, opens the blood arteries in the brain and permits inflammatory cells to enter the central nervous system (CNS).
What is the epsilon toxin?
Dr. Barbara Giesser stated that the researchers “investigated how the toxin induced an MS-like condition in a mouse model using unique and sensitive techniques to determine the presence of the bacterium.
The scientists collected faeces from both MS patients and healthy controls. They used polymerase chain reaction (PCR) analysis to examine these samples in order to find the epsilon toxin (ETX) gene, which is only present in C. perfringens.
They discovered that the ETX gene was present in 61% of samples from MS patients but only in 13% of those from healthy controls. Also, they discovered that compared to age- and sex-matched healthy controls, MS patients had a higher likelihood of having ETX-positive C. perfringens invade their gut microbiome.
Treatments to target this toxin
The current amount of knowledge regarding the gut microbiome in MS patients is expanded upon by this study. It has been demonstrated to respond to treatment with various disease-modifying treatments and is known to differ from those of non-MS controls, according to Dr. Barbara Giesser.
Epsilon toxin is only produced by C. perfringens during the rapid development phase. The researchers hypothesise that ETX is the cause of MS lesions, which would explain why the illness is episodic and manifests less symptoms when the toxin-producing bacteria are absent.
They draw the conclusion that the bacterium, its toxin, and MS exhibit a robust clinical connection. According to Dr. Giesser, this finding raises the prospect of therapies that target this pathway:
“The toxin facilitates central nervous system access for immune cells. This implies that medications that target the bacterium or the toxin may be effective in treating the condition.
The researchers point out that clinical trials would be required to see whether this could result in MS treatments.
Healthy microbiome
The development of MS may be significantly influenced by the gut microbiome, according to studies. An analysis of multiple research published in 2017 discovered that nutrition might be used to alter the gut flora and alter the course of MS.
The advantages of keeping a healthy gut microbiota are becoming more widely understood, and this study provides more proof that an unbalanced microbiota may lead to the onset of disease.
A healthy diet and lifestyle that promote the growth of advantageous gut flora may potentially lower the risk of MS as well as the risk of many other illnesses.
Improve gut health
Some elements, such as genetics and environment, are beyond your control. Although our gut microbiota is set up early in life, there are some things that can change it.
Certain modifications enhance the diversity and health of our microbiome. Alterations may be harmful.
These are some actions you may do to encourage a balanced, healthy gut microbiome:
- Consume more fibre. All of the little microorganisms in your gut can eat fibre. Fruits, vegetables, beans, lentils, nuts, seeds, and whole grains all contain fibre.
- Drink less alcohol. There is evidence that alcohol causes dysbiosis. You might want to think about reducing your drinking if you do.
- Consume fermented food. Foods that have been fermented are sources of good bacteria and may be beneficial to health. Among the foods that are fermented include kimchi, tempeh, yoghurt, kefir, miso, and sauerkraut.
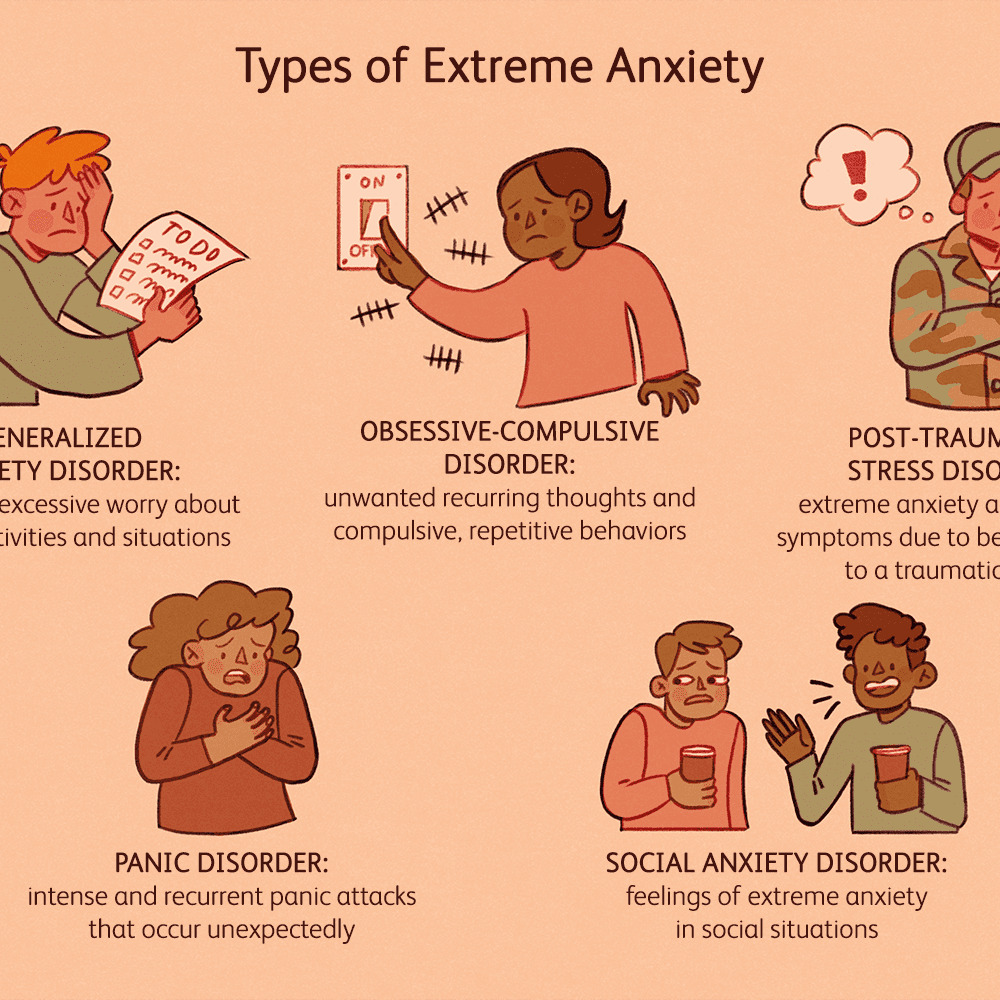
- Stress management. Your gut microbiota’s state of health can be impacted by stress. To manage tension, try some stress-relieving exercises like yoga or meditation.
- Don’t overuse antibiotics. Antibiotics can kill some of the helpful bacteria in addition to the harmful ones. Dysbiosis may result from this. Antibiotics should only be used as necessary, and they should be taken exactly as prescribed. Some of the beneficial bacteria may be restored by taking a probiotic supplement.
- Look into probiotic dietary supplements. Supplements with probiotics may be beneficial. To determine the appropriate dosage and strain for particular ailments, more research is required. Start with the US Probiotic Guide if you want to.
Conclusive note
- The human body is home to trillions of microorganisms. The gut contains the majority of them.
- The possibility that the sorts of bacteria in our guts may have an impact on our health is intriguing.
- Dysbiosis is more likely to occur in MS patients. When the gut microbiota is out of equilibrium, it is called dysbiosis. Inflammation and autoimmune illnesses are now more likely as a result.
- A healthy gut microbiota can be supported by consuming fermented foods and a high-fiber diet.
- There is continuing research into the potential benefits of altering the gut microbiome for MS patients.
REFERENCES:
- https://www.healthline.com/health/ms/link-between-ms-and-gut
- https://www.medicalnewstoday.com/articles/toxin-from-gut-bacteria-may-trigger-multiple-sclerosis-onset-and-relapse
- https://www.hpnonline.com/surgical-critical-care/article/53056101/bacterial-toxin-may-trigger-ms-onset-and-relapse
- https://www.medicaldaily.com/toxin-gut-bacteria-may-trigger-multiple-sclerosis-study-suggests-469268
For more details, kindly visit below.