Japanese Diet May Slow Progression Of Fatty Liver Disease.
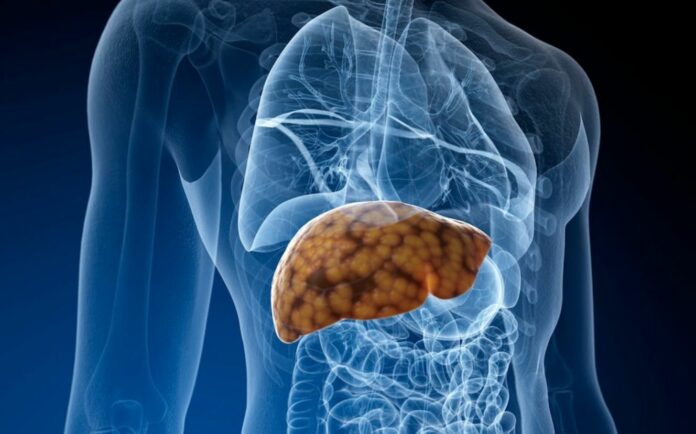
According to a new study, a Japanese diet can reduce the progression of non-alcoholic fatty liver disease in those who already have the condition.
According to the study, soy products, shellfish, and seaweed have the strongest links to slowed liver fibrosis progression. The Japanese diet encourages eating high-quality foods and consuming less sodium, sugar, and saturated fat.
According to a recent study, persons with non-alcoholic fatty liver disease (NAFLD) may be able to reduce the illness’s progression by adopting a Japanese-style diet.
136 patients with NAFLD were being treated at the Osaka Metropolitan University Hospital in Japan when the study’s authors followed their diet and the development of their illness.
Each person’s diet was evaluated by researchers based on how closely it adhered to the 12-component Japanese Diet Index or mJDI12. High mJDI12 scores were linked to a slowing of the NAFLD-related liver fibrosis development.
There are 12 different foods and dietary groups in the Japanese diet:
- rice
- Miso broth
- pickles
- soy-based goods
- yellow and green vegetables
- fruits
- seafood
- mushrooms
- seaweed
- emerald tea
- coffee
- pork and beef
About the Japanese diet, those who ate more soy, seafood, and seaweed experienced the greatest inhibition of the development of liver fibrosis.
The impact of food on muscle mass was also monitored by the researchers. They discovered that individuals who consumed more soy products did so in addition to having lower rates of fibrosis advancement.
What precisely is non-alcoholic fatty liver disease?
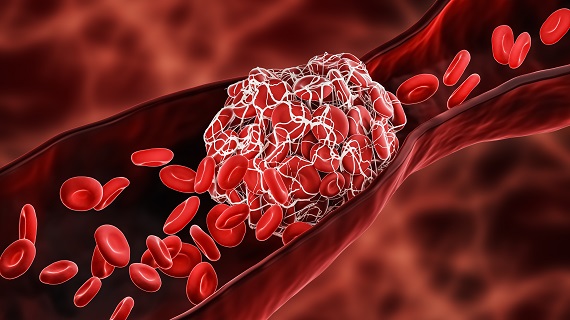
Although it doesn’t directly harm the liver, NAFLD is a condition in which fat deposits there can potentially affect how well the organ functions.
The risk of non-liver malignancies, such as colon cancer, chronic kidney disease, gastric reflux, obstructive sleep apnea, hypothyroidism, periodontitis, polycystic ovarian syndrome, psychiatric issues, and growth hormone issues, is increased in those with NAFLD.
To better understand how the disease progresses, we spoke with Dr. Muhammad Nadeem Aslam, an assistant research scientist in the Department of Pathology at the University of Michigan who was not involved in the study.
Utilizing excessive amounts of fat, especially saturated fat, processed carbohydrates like fructose, glucose, and sucrose. Also, consuming too many calories, causes an imbalance between fat accumulation and breakdown in the liver, with the result being fat buildup in the liver.
Dietitian for heart health Michelle Routhenstein, who was also excluded from the study, stated:
“Foods high in refined sugars, saturated fat, salt, or trans fat can all contribute to fatty liver disease. This is done by causing the body to become more oxidatively stressed and inflammatory.”
While fatty infiltration is typically tolerated, Dr. Aslam added that an excessive buildup of lipids in the liver. This includes triglycerides, free fatty acids, and cholesterol, which can cause cellular stress and the production of reactive oxygen species.
According to Rosenstein, some items that encourage NAFLD include hydrogenated oils, fried foods, drinks, soda, and processed foods.
What makes Japanese cuisine wholesome?
Fresh, unadulterated foods with little refined ingredients, saturated fats, and added sugar make up the majority of the Japanese diet.
Due to their diet’s high soy and fish content, previous studies have shown that those who follow the Japanese diet had a lower risk of cardiovascular disease and stroke.
The largest population of centenarians is found on the island of Okinawa, which is located in southernmost Japan. The extended life expectancy and decreased incidence of obesity among Japanese people may be due to their low-calorie, nutrient-dense diet.
According to studies, Japanese people have the lowest risk of developing age-related illnesses such as diabetes, cancer, arthritis, and Alzheimer’s.
Some advantages of the Japanese diet include the following:
It enhances digestion – Fiber-rich foods that help with digestion include fruits, vegetables, seaweed, soybeans, and soy products. Fruits and vegetables that have been pickled are a wonderful source of probiotics.
It is a nutrient-rich diet – Japanese cuisine naturally contains a lot of minerals, vitamins, and nutrients including omega-3 fats.
Natural low-calorie foods and the Japanese practice of eating until 80 percent full assist prevent overeating. Also, provide the calorie deficit necessary for weight loss, which contributes to maintaining a healthy weight.
The Japanese eating style, in addition to the food, aids in keeping good health. The senses are stimulated when food is consumed from a tiny bowl with numerous different dishes rather than a large plate. They adhere to the “flexible restraint” philosophy, which permits occasional small-portion consumption of snacks and treats.
The following three Japanese foods
The study’s top three foods each have their own advantages, but they also have at least one thing in common: they are low in fat. Dr. Aslam cited soybeans as an example of a plant protein that is high in fiber and low in saturated fat.
Given that soy is a complete protein that contains all necessary amino acids to support the synthesis of muscle proteins, soy is “associated with higher muscle mass,” according to Rosenstein.
“Seafood, especially fish, is a good source of vitamins D and B2 (riboflavin), as well as omega-3 fatty acids. In addition to being a fantastic source of minerals like iron, zinc, iodine, magnesium, and potassium, fish is also high in calcium and phosphorus, according to Dr. Aslam.
According to Routhenstein, seafood may have a suppressive influence on the evolution of fibrosis because of its anti-inflammatory and antioxidant qualities.
Japanese seaweed is a good source of vitamins, minerals, and polyphenols. Dr. Aslam continued, “In addition to vitamins, the majority of edible algae have a special blend of nutrients.
Additional foods that lower NAFLD
The Mediterranean diet is another eating plan with a good reputation for helping those with NAFLD. Lean meats, fruits, vegetables, nuts, legumes, whole grains, and other plant-based foods are highlighted.
According to Routhenstein, green tea is one food in the mJDI12 index that is particularly beneficial for NAFLD because of its antioxidant content.
It “is protective against fatty liver disease because it contains about 200-300 mg of epigallocatechin-3-gallate (EGCG) in one cup,” claimed Routhenstein.
Dr. Aslam noted that coffee beans high in antioxidants are also linked to a generally lower risk for NAFLD.
“Raspberries are rich in insoluble fiber that helps create a short chain fatty acid in the gut called butyrate which studies have shown to be helpful in the reversal and prevention of fatty liver disease,” Routhenstein noted.
Including Japanese food and culture in one’s diet
This study highlights the chance to take charge of your health by including therapeutic foods to help stop the advancement of fatty liver disease, according to Routhenstein.
Dr. Aslam voiced alarm over the fact that so many Americans continue to consume a diet that is “far below dietary guidelines recommendations for healthy dietary patterns.”
“The lack of these nutrient-dense foods in the daily diets can cause diet-related chronic diseases, such as cardiovascular disease, type 2 diabetes, obesity, and fatty liver disease,” claimed Dr. Aslam.
Dr. Aslam praised nutrient-rich diets, which are lower in sodium, sugar, and saturated fat:
“Nutrient-dense foods are those that are prepared with no or little added sugars, saturated fat, and sodium,” said Dr. Aslam. “These foods include vegetables, fruits, whole grains, seafood, eggs, beans, peas, and lentils, unsalted nuts and seeds, fat-free and low-fat dairy products, and lean meats and poultry.”
REFERENCES:
- https://www.medicalnewstoday.com/articles/the-japanese-diet-may-slow-the-progression-of-fatty-liver-disease
- https://www.medicaldaily.com/japanese-diet-may-slow-progression-fatty-liver-disease-3-foods-that-suppress-liver-fibrosis-469634
- https://www.express.co.uk/life-style/health/1765674/fatty-liver-disease-japanese-diet
For Alzheimer’s disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?generic=192