Scientists spot brain changes that may help predict stages of dementia
This is a significant and active area of research. Here’s a detailed breakdown of how scientists are spotting brain changes to predict the stages of dementia, moving from established methods to cutting-edge advances.
The Core Concept: Predicting Progression, Not Just Diagnosing
The key shift in modern dementia research is moving from a diagnosis based on clear symptoms to a predictive model. The goal is to identify the underlying disease process (like Alzheimer’s pathology) years or even decades before significant cognitive decline occurs, and then track its progression through predictable stages.
The most influential framework for this is the AT(N) Framework for Alzheimer’s disease, which classifies biomarkers into three categories:
- A: Amyloid-beta pathology
- T: Tau pathology
- (N): Neurodegeneration or neuronal injury
Scientists use a combination of tools to measure these.
1. Key Brain Changes and the Tools to Spot Them
A. Amyloid-Beta Plaques (The “A” in AT(N))
- What it is: Sticky protein fragments that clump together outside neurons, forming plaques. This is a hallmark of Alzheimer’s.
- How it’s Spotted:
- PET Scans (Amyloid-PET): A radioactive tracer binds to amyloid plaques in the brain, making them visible on a scan. A positive scan indicates amyloid accumulation, a key early risk factor.
- Cerebrospinal Fluid (CSF) Analysis: A lumbar puncture can measure the levels of amyloid in the spinal fluid. Low levels of amyloid-42 in the CSF indicate that the protein is being trapped in the brain as plaques.
B. Tau Tangles (The “T” in AT(N))
- What it is: Twisted fibers of a protein called tau that build up inside nerve cells, disrupting their transport system and eventually killing them. The spread of tau tangles is more closely correlated with the severity of cognitive decline.
- How it’s Spotted:
- PET Scans (Tau-PET): Newer tracers can now make tau tangles visible. This is a major breakthrough. Researchers can see where tau is building up and track its spread from memory centers to other brain regions, which predicts the transition from mild cognitive impairment (MCI) to full dementia.
- CSF Analysis: Elevated levels of phosphorylated-tau (p-tau) in the spinal fluid are a direct marker of tau tangle pathology.
C. Brain Structure and Metabolism (The “N” in AT(N))
- What it is: The downstream effects of amyloid and tau—actual brain cell death and loss of function.
- How it’s Spotted:
- MRI (Magnetic Resonance Imaging):
- Volume Loss (Atrophy): MRI can precisely measure the shrinking of specific brain regions. In Alzheimer’s, early shrinkage is seen in the hippocampus and entorhinal cortex (critical for memory). The rate of atrophy can predict how quickly the disease will progress.
- Connectivity: Advanced MRI can track the weakening of connections between different brain networks.
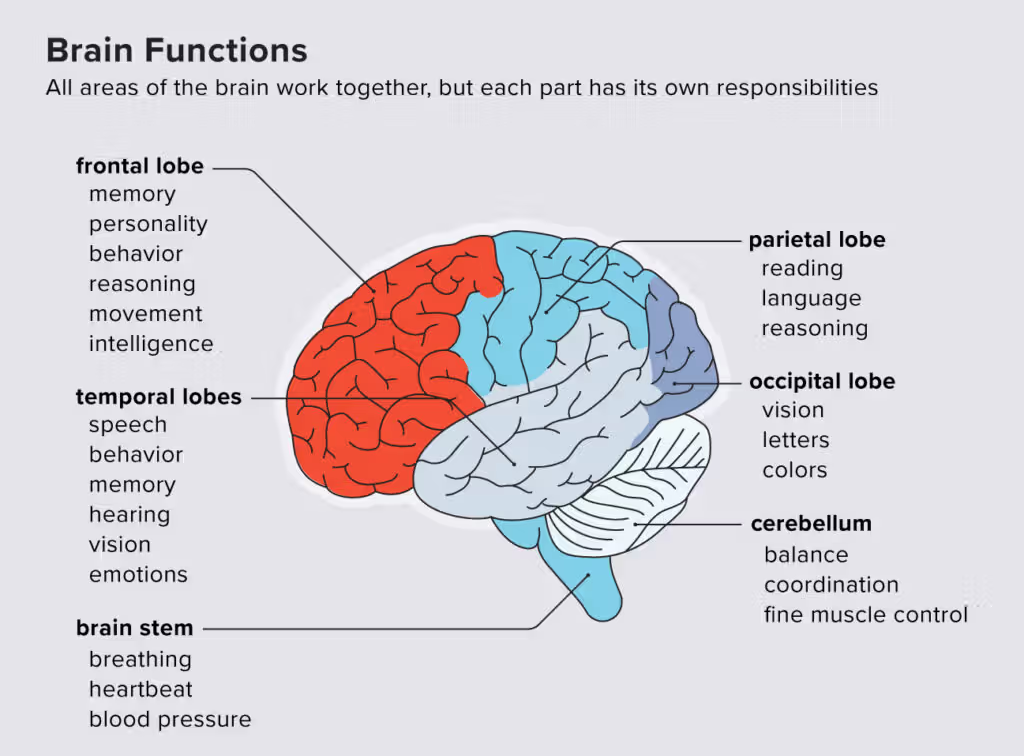
- FDG-PET Scans: This scan measures glucose metabolism. Brain cells affected by dementia are less active and consume less sugar, showing up as “dark” or “cold” spots on the scan. A pattern of reduced metabolism in the parietal and temporal lobes is a classic predictor of Alzheimer’s progression.
- MRI (Magnetic Resonance Imaging):
D. A New Frontier: Blood-Based Biomarkers (Liquid Biopsy)
This is one of the most exciting recent developments. Scientists have developed highly sensitive blood tests that can detect minute levels of:
- p-tau217 and p-tau181: These are specific forms of tau that are highly accurate in identifying Alzheimer’s pathology, even distinguishing it from other dementias.
- Amyloid Ratios: Blood tests can now predict amyloid status in the brain with over 90% accuracy.
Why this is a game-changer: Blood tests are far cheaper, less invasive, and more scalable than PET scans or lumbar punctures, making them ideal for widespread screening and clinical trials.
2. How These Changes Map to Stages of Dementia
By combining these biomarkers, researchers can create a predictive timeline:
| Stage | Clinical Presentation | Key Brain Changes (Biomarkers) |
|---|---|---|
| Preclinical | No symptoms. The person functions normally. | Amyloid begins to accumulate (positive Amyloid-PET or low CSF Aβ42). Tau may start to appear. This stage can last 10-20 years. |
| Mild Cognitive Impairment (MCI) due to Alzheimer’s | Mild, noticeable symptoms (e.g., forgetting recent conversations, getting lost), but not severe enough to interfere significantly with daily life. | Tau spreads significantly, especially in memory regions. Neurodegeneration begins (hippocampal shrinkage on MRI, reduced metabolism on FDG-PET). |
| Dementia due to Alzheimer’s | Significant cognitive decline that impairs daily activities (managing finances, driving, personal care). | Widespread tau pathology throughout the cortex. Significant and spreading brain atrophy. Marked hypometabolism. |
The Future and Implications
- Early Intervention: The ultimate goal is to identify people in the preclinical or MCI stage and treat them with disease-modifying therapies (like lecanemab and donanemab) that clear amyloid or target tau, before widespread brain damage occurs.
- Personalized Prognosis: Doctors will be able to provide a more accurate prognosis by looking at an individual’s specific biomarker profile (e.g., “You have high amyloid and tau in region X, suggesting a higher risk of progression within 2 years”).
- Improved Clinical Trials: These biomarkers allow researchers to enroll the right participants for trials (those with the underlying pathology) and use biomarker changes as endpoints to see if a drug is working, much faster than waiting for cognitive scores to change.
Conclusion
Scientists are no longer just looking at a static picture of a “demented brain.” They are now using a dynamic toolkit of Amyloid-PET, Tau-PET, MRI, and blood tests to track the sequence of pathological events. This allows them to predict the risk, diagnose the specific stage, and forecast the likely progression of diseases like Alzheimer’s with ever-increasing precision, opening the door to a future where dementia can be slowed or prevented.
Medications that have been suggested by doctors worldwide are available on the link below
https://mygenericpharmacy.com/category/products/mens-health