Epilepsy risk is 2.5 times higher in hypertensive people.
Researchers looked into the connection between epilepsy and high blood pressure. They discovered that taking antihypertensive drugs lowers the risk of epilepsy. This is increased by high blood pressure by about 2.5 times.
They come to the conclusion that while high blood pressure is a risk factor for epilepsy, further research is required to fully understand the mechanisms that underlie the association.

After stroke and dementia, epilepsy is the third most prevalent neurological illness that affects elderly individuals.
According to research, late-onset epilepsy has increased in prevalence over the past 20 years. As the population ages, the prevalence of the disorder will undoubtedly continue to climb. This makes epilepsy a substantial public health concern.
Despite this, 32-48% of cases of epilepsy have unknown underlying causes. According to several studies, vascular risk factors may raise the chance of developing late-onset epilepsy. According to another study, epilepsy may be caused by vascular risk factors starting in a person’s 30s.
Policymakers may be better able to develop public health initiatives and preventive actions to lower and manage rates of the condition if they have a better understanding of the involvement of vascular risk factors in late-onset epilepsy.
A recent investigation of the relationship between vascular risk factors and the start of epilepsy was conducted by researchers in the United States under the direction of the Boston University School of Medicine.
They discovered a connection between hypertension and a nearly 2-fold increased incidence of late-onset epilepsy. For those who did not use medication to control their blood pressure, this risk was significantly larger.
Data evaluation
Data from the Framingham Heart Study (FHS), an ongoing, community-based study that started in 1948, was used by the researchers. Through health exams every four years, the Offspring Cohort follows the health outcomes of 5,124 of the children of the original participants.
The researchers combined data from 2,986 individuals who underwent their fifth checkup between 1991 and 1995, were at least 45 years old at the time, and whose health records contained information on vascular risk factors.
Systolic and diastolic blood pressure were measured as vascular risk factors. The researchers defined high blood pressure as having a systolic pressure of at least 140 millimeters of mercury (mm Hg) and a diastolic pressure of at least 90 mm Hg, as well as taking antihypertensive drugs.
Additionally, the researchers looked for:
- diabetes
- cholesterin amounts
- smoking history
- a cardiovascular condition
- stroke
- BMI, or body mass index
The ICD-9 codes associated with epilepsy or seizures, self-reported seizures, routine chart reviews for neurological diseases, and antiepileptic medication use were utilised by the researchers to screen participants for epilepsy or seizures.
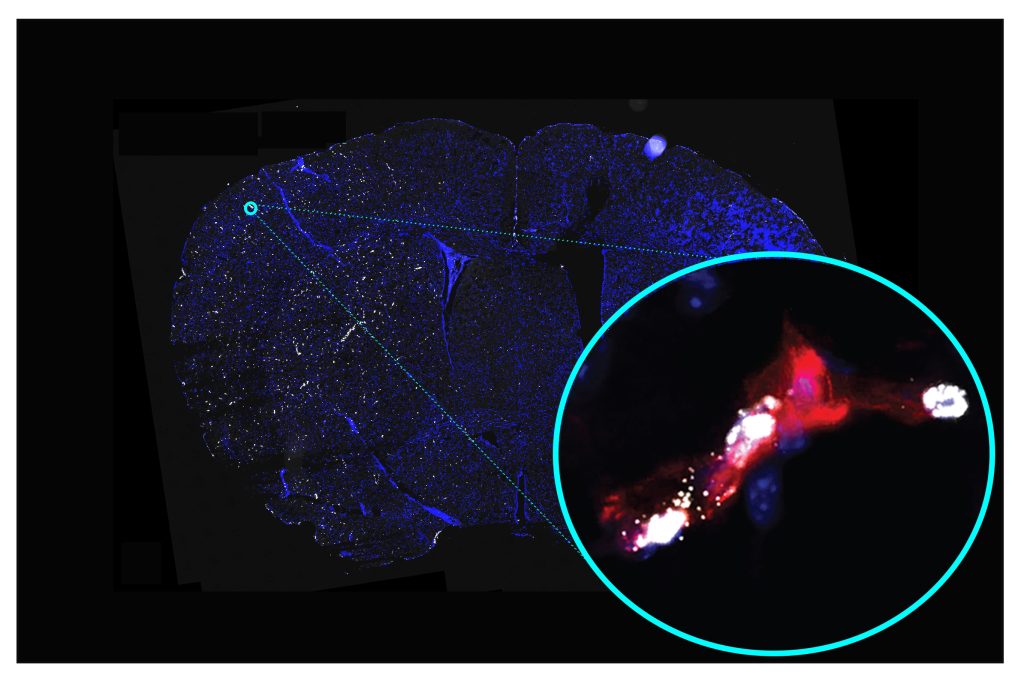
To identify cases of epilepsy, the researchers also analysed electroencephalography (EEG), cardiac, and other pertinent data, as well as brain imaging.
The study found 55 cases of epilepsy in the group, of which 26 were confirmed, 15 were likely, and 14 were suspected. The average age of the subjects at the time of a possible diagnosis was 73.8 years old.
The study’s findings revealed a nearly 2-fold increased risk of epilepsy in people with hypertension. The other risk variables, however, were unrelated to epilepsy.
They also discovered that the probability of having epilepsy increased by 17% for every 10 mm Hg change in systolic blood pressure.
Underlying processes
The connection between epilepsy and hypertension is explained by several theories. The renin-angiotensin system (RAS), which controls blood pressure, may be one mechanism.
According to research, rats who have had repeated seizures had 2.6–8.2 times the RAS components of seizure-free mice. Antihypertensive medications that decreased RAS component levels postponed the start of seizures and decreased their frequency.
More investigation is required, though, as other studies indicate the system may only have a modest impact on the relationship between epilepsy and hypertension.
Small vascular disease (SVD), a disorder in which the walls of small arteries and capillaries are damaged and do not adequately convey oxygen-rich blood to numerous organs, is another potential underlying mechanism, claim the researchers. According to a recent study, the duration of high blood pressure is a reliable indicator of developing SVD in later life.
The researchers also mention that temporal lobe epilepsy and SVD are related. Cortical microinfarcts, tiny lesions in the cortical tissue, and the disruption of U fibers are a few potential explanations. These conditions may cause excessive excitability and hence seizures. U fibers link adjacent regions of the cerebral cortex.
The researchers draw the conclusion that hypertension is a standalone predictor of late-onset epilepsy and carries a 2-fold chance of getting seizures after 45 years.
They do acknowledge that their study has some limitations. It might not accurately represent all races and ethnicities because it was mostly made up of white people. The study’s observational design, according to the researchers, precludes the ability to establish causality.
Dr. Jason Hauptman, a neurosurgeon at Seattle Children’s Hospital, told us that these findings were particularly intriguing because there has been debate over whether elevated blood pressure (hypertension) is a standalone risk factor for stroke.
living with high blood pressure and epilepsy
A healthy blood pressure reading is less than 120/80 mmHg; if you are unsure of your current blood pressure, ask your doctor. High blood pressure is closely linked to a variety of health risks, including cardiac arrest, so it is important to try and maintain this level. The good news is that there are lots of easy lifestyle adjustments you can make to lower your blood pressure, like:
- healthy eating
- not a smoker
- controlling stress
- lowering the consumption of alcohol
- Exercising
- consuming less salt
Speak to your doctor if you have concerns about your epilepsy and high blood pressure. They can assist you in creating a management strategy to lower your blood pressure through dietary and activity modifications. while also making sure that you are controlling your seizures.
REFERENCES:
- https://www.medicalnewstoday.com/articles/hypertension-linked-to-2-5-times-higher-risk-of-epilepsy
- https://hartfordhealthcare.org/about-us/news-press/news-detail?articleid=37975&publicId=395
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8078946/
- https://www.epsyhealth.com/seizure-epilepsy-blog/blood-pressure-and-epilepsy-an-overview
For Epilepsy disease treatments that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=49