Depression increases the risk of mortality among people living with diabetes
More than 462 million people worldwide suffer with type 2 diabetes, making it the ninth most common cause of death. People with type 2 diabetes frequently experience mental health problems; research indicates that the likelihood of depression is twice as high in those with the disease as in those without it. According to a recent study, the risk of dying young is four times higher for those who have type 2 diabetes and depression combined than for those who don’t. The authors advocate for the inclusion of mental health services in type 2 diabetes patients’ medical regimens.
Using data from the Global Burden of Disease dataset, a study conducted in 2017 projected that 462 million individuals worldwide, or 6.28% of the total population, had type 2 diabetes. Since then, the number has grown, and by 2050, it is anticipated that there will be more than 1.3 billion type 2 diabetics globally. Individuals who have diabetes are more likely than those who do not to experience depression. The World Health Organization (WHO) estimates that 5% of persons worldwide suffer from depression, also known as depressive disorder. Research has also shown that people with type 2 diabetes have twice the risk of developing depression compared to the general population.
Type 2 diabetes and depression together can raise the chance of death by up to four times, according to a recent study. Both illnesses increase the risk of mortality. Professor of public health at current Mexico State University and lead and corresponding author of the current study Dr. Jagdish Khubchandani told MNT that “it is estimated that almost a fifth of people with diabetes may also have depression symptoms of varying severity” globally. Data from 14,920 participants in the National Health and Nutrition Examination Survey, conducted between 2005 and 2010, were analyzed by the researchers. The Centers for Disease Control and Prevention (CDC) death records up to December 31, 2019, were then linked to these data.
When it came to the participants’ diabetes status, the researchers recorded it as diabetes if they replied “yes” or “borderline” to the question, “Other than during pregnancy, have you ever been told by a doctor or other health professional that you have diabetes or sugar diabetes?”. They measured depression using the PHQ-9, a tool for gauging depression severity. Anyone who received a score of 10 or higher on the questionnaire—which has a maximum score of 27—was deemed to have depression. 10% of the cohort had type 2 diabetes, and 9 points08 percent had depression. Sixteen percent of people with type 2 diabetes also experienced depression. The researchers discovered that, overall, individuals with type 2 diabetes had a 1:7 chance of dying before their time after adjusting for sociodemographic variables. The risk of dying young was more than four times higher for those with type 2 diabetes and depression than for those without either illness.
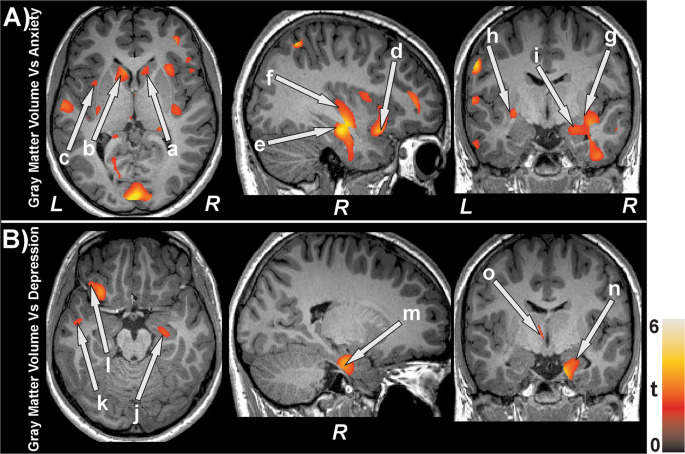
“Considering the range of additional conditions, including depression, that often coexist with diabetes, specialists in diabetes care may not be able to provide assistance on their own,” he continued. Dr. This viewpoint was echoed by Gabbay, who stated that “[t]he American Diabetes Association Standards of Care recommends routine screening for depression because it is a common condition in people with diabetes, predicts poor outcomes, and, shockingly, now increases the risk of death.”. “It is crucial to screen for depression, which can be as easy as asking a PHQ-2 question [about the frequency of depressed mood], and then concentrate on appropriate treatments, given that there are effective treatments for depression,” he said. According to Dr. Gabbay, there are a number of factors that may contribute to diabetes and depression, including inflammation, sleep disturbance, an inactive lifestyle, poor dietary habits, and environmental and cultural risk factors.
There are several possible explanations for the link between type 2 diabetes and depression. He pointed out that people who are depressed are frequently less likely to lead healthy lifestyles, which can result in poorer glucose regulation and an increased risk of diabetes complications. We may not fully understand the biological connection, but it appears to play a significant role in the relationship between depression and type 2 diabetes, Dr. Gabbay continued. Dr. Khubchandani stressed how critical it is to treat both illnesses. He informed us that a combination of antidepressants and hypoglycemic drugs are recommended for optimum management of both the disorders and to prevent worsening of any of these, although receiving treatment for any one of the two disorders is still preferable to receiving none at all. He continued, Frequent monitoring and screening is essential for this to occur, and diabetes care practitioners must remain vigilant about mental health issues among patients.. Dr. Khubchandani further emphasized the need for prompt action to stop needless diabetes-related deaths. He emphasized that by 2050, the number of people with diabetes worldwide will have rapidly doubled from 400 million today, adding that diabetes imposes a lot of social, economic, and emotional burdens.. In the absence of a more thorough and serious approach to mental health issues, the number of diabetics who pass away too soon will increase. .
High blood sugar levels brought on by diabetes can cause a number of health problems that can impact the body’s organs. Controlling these levels can lower the chance of harm occurring to the entire body. Diabetes can be treated to a lesser extent by receiving an early diagnosis and adhering to a treatment plan that includes medication, lifestyle modifications, and routine medical care. The primary cause of early death for diabetics is cardiovascular disease, according to the Centers for Disease Control and Prevention (CDC). According to the CDC, the risk of having a stroke or passing away from heart disease is two to three times higher for those who have diabetes than for those who do not. Moreover, diabetes patients typically experience more severe cardiac issues earlier in life than non-diabetic individuals. Furthermore, diabetes frequently coexists with other heart-stressing conditions like obesity, hypertension, and high cholesterol. Diabetes and cardiovascular disease are both at risk due to poor diet and inactivity. When there is an infection or wound, the body’s capacity to heal is compromised by poor circulation. The lack of blood, oxygen, and nutrients is the cause of this. Diabetes patients should frequently examine their skin for wounds and should consult a physician if they experience any infection-related symptoms, such as redness, swelling, or fever.
One of the most frequent side effects of diabetes is neuropathy, or nerve damage. Nerve damage affects roughly 10–20% of individuals with diabetes at diagnosis. A person’s risk of developing neuropathy increases with the length of time they have diabetes. Over 50% of individuals with diabetes will develop the illness at some point. Any area of the nervous system, including the nerves governing autonomic or involuntary processes like digestion, can be affected by neuropathy. On the other hand, peripheral neuropathy is the most prevalent type. The legs, feet, and toes, as well as the arms, hands, and fingers, are affected, resulting in pain and numbness. The upper legs and hips can also be affected by neuropathy. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), peripheral neuropathy accounts for up to 50% of cases of diabetes, while autonomic neuropathy accounts for over 30% of cases. High blood sugar levels have the potential to harm kidney blood vessels over time. The kidneys’ ability to filter waste from the blood is compromised by this damage. Kidney failure may develop eventually. One of the primary causes of kidney disease, according to the NIDDK, is diabetes. It impacts one in three diabetics.
Diabetes raises the possibility of several ocular issues, some of which can result in blindness. One of the short-term issues is hazy vision from elevated blood sugar. Diabetic retinopathy, macular edema, cataracts, and glaucoma are long-term complications. Controlling blood sugar, avoiding or quitting smoking, and scheduling routine eye exams can all help preserve eye health in diabetics. Nervous system damage can impact autonomic bodily processes, such as digestion. When nerve damage prevents the digestive system from properly moving food from the stomach into the small intestine, the condition known as gastroparesis may result. Diabetes may cause a person to experience nausea, vomiting, acid reflux, bloating, abdominal pain, and, in extreme situations, weight loss. Stress can be reduced by learning as much as possible about diabetes. It may also cause concerns about treatment, health, and potential complications that can lead to stress, anxiety, and depression. Concerns about the cost of treatment and whether or not they are getting it right, especially if symptoms change mood disorders that make it difficult for a person to maintain a healthy lifestyle. A person will feel more in control of their diabetes and its management the more informed they are about their illness. Being aware of what to do in every circumstance can help someone feel more confident and better about themselves in general. Reducing these issues can be achieved by collaborating with a healthcare provider. A physician or therapist may do so.
REFERENCES:
For Anti Depression and Diabetes medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=30