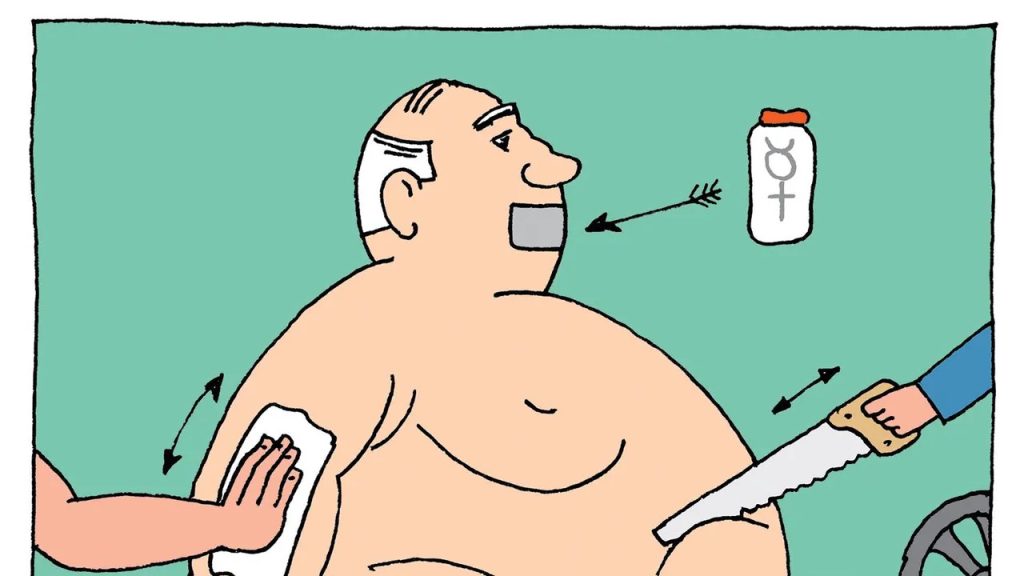
Exercise & weight loss can improve obesity and prediabetes.
According to new research, people who are overweight and have prediabetes may benefit significantly from regular exercise when accompanied with weight loss via diet.
The goal of the study was to ascertain whether exercise had benefits in addition to those provided by diet-only weight loss.
The study examined two groups, one of which followed a diet plan plus exercise training and the other of which followed a diet plan alone.

According to the findings, the group that combined diet and exercise improved their insulin sensitivity by twice as much as the diet-only group, which is essential for controlling prediabetes.
Researchers from the Centre for Human Nutrition at Washington University School of Medicine in St. Louis, Missouri, examined the results of regular exercise paired with a nutrition programme for people in a recent study.
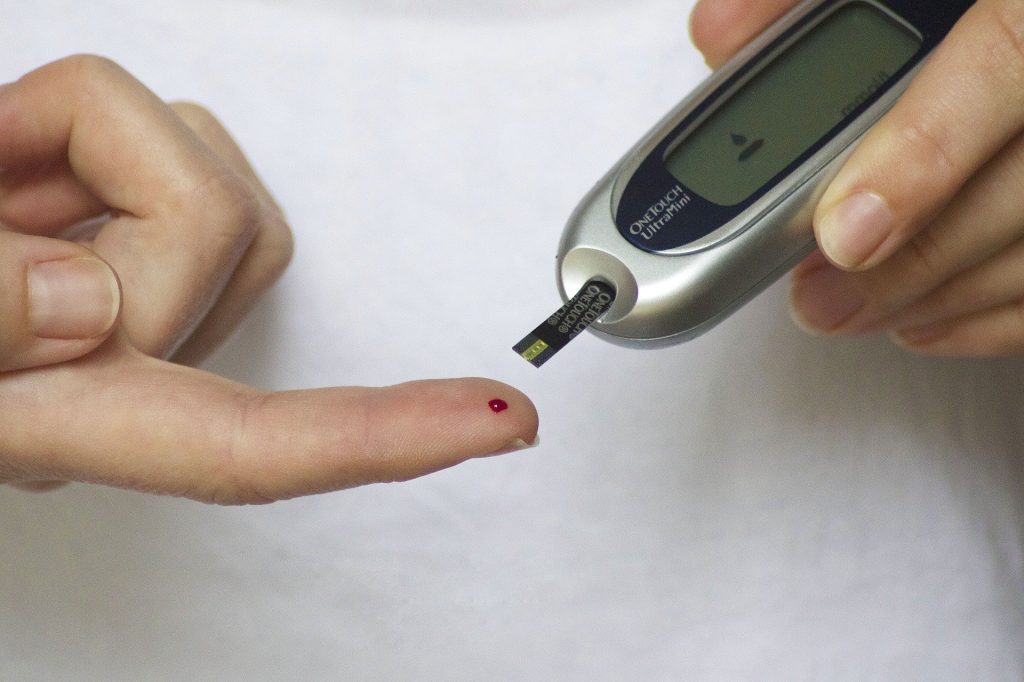
The individuals’ bodies’ sensitivity to the hormone insulin, which regulates blood sugar levels, was tested by the researchers.
According to the findings, those who made changes to their eating and exercise routines saw a twofold increase in their insulin sensitivity compared to those who only made dietary changes.
This indicates that their bodies used insulin to regulate blood sugar levels more effectively.
The participants’ muscles were also examined by the researchers, and they discovered that the group that changed their diet and exercise regimens had higher expression (activity) of genes related to the production of new mitochondria, which are cells’ energy factories, energy metabolism, and the development of new blood vessels.
They discovered no discernible differences between the two groups in terms of the amounts of specific amino acids or particular inflammatory blood indicators.
The composition of their gut bacteria also changed similarly in both groups, which can have an impact on general health.
Exercise for managing and treating obesity
We spoke with Dr. Sergio P. Ramoa of Atrius Health, who was not a part of the study, and he stated that “despite the growing focus and treatment of obesity and diabetes, diabetes-related mortality increased in the first 20 years of the 21st century.”
“The approach to treating obesity has altered, with a focus on treating it like a chronic illness like hypertension or asthma. There have been considerable advancements in the treatment of weight reduction and weight maintenance, according to Dr. Sergio P. Ramoa, as a result of changes in social, educational, and therapeutic attitudes.
In his statement, Dr. Romoa said that “This article demonstrates why exercise continues to be a pillar of not only weight management treatment but the overall health of the community.”
“Exercise should always be used in conjunction with pharmaceutical treatment for persistent lifestyle changes,” he advised.
The National Coalition on Healthcare’s (NCHC) Kelsey Costa, a registered dietitian and health research specialist who was not involved in the study, concurred, saying that “the study findings imply that combining exercise training with a calorie-restricted diet can enhance insulin sensitivity and metabolic health beyond the benefits achieved solely through diet-induced weight loss.”
As Costa said, “It is essential to understand how effectively this combination of therapies can improve metabolic health given what we know about the barriers to exercise in people with obesity.”
For managing prediabetes, insulin sensitivity is essential.
Prediabetes is characterized by persistently elevated blood glucose levels that are not yet high enough to progress to type 2 diabetes.
Although it acts as a warning sign for an elevated risk of getting diabetes, it is frequently preventable or deferred with lifestyle adjustments.
Enhancing insulin sensitivity through exercise
According to Dr. Romoa, “GLUT4, the main insulin-driven glucose transporter, exercise improves insulin sensitivity.”
“GLUT4 is present in adipose and muscular tissue. The amount of these transporters varies depending on a person’s diabetes and obesity condition.
While they drop in adipose tissue, they hold steady in muscular tissue. As a result, exercise can keep enhancing glucose regulation. Due to insulin resistance, adipose tissue can no longer adequately regulate blood glucose. Additionally, exercise will increase the body’s GLUT4 levels. Walking can help lower blood sugar levels, according to Dr. Sergio P. Ramoa.
It was said by Costa that this study showed that “exercise enhances insulin-stimulated glucose uptake, likely due to changes in skeletal muscle biology induced by exercise.”
This includes an improvement in mitochondrial content and function as well as an increase of genes related to substrate oxidation and mitochondrial energy metabolism. The diet plus exercise group consequently saw a more significant rise in muscle insulin sensitivity,” Costa said.
Type 2 diabetes treatment through exercise
Exercise is strongly advised as a main treatment for type 2 diabetes, according to prior research.
Combining 150 minutes per week of moderate to strenuous exercise with dietary and behavioural adjustments can stop, delay, or even reverse the condition.
Exercise of all kinds, including resistance and aerobic training, can regulate blood sugar levels. Small bursts of exercise spread out throughout the day and high intensity interval training are both good.
Exercise in the afternoon or right after a meal, for example, may have additional benefits.
Exercise guidelines that are ideal Working with healthcare experts is crucial for personalised diabetes management because individual aspects are continuously being researched.
Costa stressed “the significance of integrating a calorie-restricted diet with exercise training to enhance metabolic health and physical function.”
Exercise caution
Be sure to consult your doctor before beginning a new workout routine. Make sure you drink enough water before, during, and after the activity.
To keep your blood sugar levels within the desired range, be sure to closely monitor them as well.
REFERENCES:
- https://www.medicalnewstoday.com/articles/pairing-exercise-weight-loss-can-improve-prediabetes-obesity
- https://medicalxpress.com/news/2023-06-weight-loss-combo-diabetes.html
- https://medicine.wustl.edu/news/in-battling-obesity-and-prediabetes-combining-exercise-with-weight-loss-is-key/
- https://www.healthline.com/health/type-2-diabetes/top-exercises
For Diabetes medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=13