Cardiovascular disease: Vegetarian diet might reduce risk.
Researchers looked into how vegetarian diets affected people who had a high risk of developing cardiovascular disease.
They discovered that following a plant-based diet for six months reduced various indicators of cardiometabolic risk, including blood sugar and cholesterol.
Those with a high risk of cardiovascular diseases may benefit from eating a more plant-based diet.

19.9 million people died in 2019 from cardiovascular disease (CVD), which was the cause of 32% of fatalities worldwide. For 85% of these fatalities, a heart attack or stroke was to blame.
According to studies, lifestyle variables like food, smoking, and physical inactivity frequently contribute to CVD development. Thus, lowering the incidence of CVD requires practical measures that may enhance cardiometabolic risk profiles.
A growing body of evidence suggests that adopting a vegetarian diet may help reduce cardiovascular disease (CVD). But less is known about how these diets may impact people who already have a CVD or are at high risk for developing one.
Researchers from the University of Sydney, Royal Prince Alfred Hospital, and Brescia University in Italy and Australia recently looked into how main cardiometabolic risk variables are affected by vegetarian diets in individuals with or at high risk for cardiovascular disease (CVD).
They discovered that among people at high risk of CVD, eating a vegetarian diet for six months was associated with better measurements of cholesterol, blood sugar, and body weight.
Senior clinical dietician Dr. Dana Hunnes, who was not affiliated with the study and works at the UCLA Medical Centre in Los Angeles, said the following to us:
“Vegetarian diets are better for all of us because they reduce greenhouse gas emissions, and use less water and land than non-vegetarian diets do for CVD health alone.”
The effects of nutrition on health
The American Heart Association recommends a diet that emphasises minimally processed plant foods, fish, shellfish, and low-fat dairy products as part of a balanced eating pattern. The meta-analysis examined 20 randomised controlled studies that demonstrate the value of a vegetarian diet in the general population for preventing cardiovascular illnesses.
Using randomized clinical trials, this study attempts to examine the link between a plant-based diet and cardiometabolic risk factors, according to Jenna Litt, a registered dietitian at Northwell Lenox Hill Hospital who was not involved in the research. In contrast to earlier research, this one focuses on various vegetarian diets, such as veganism versus lacto-ovo vegetarianism.
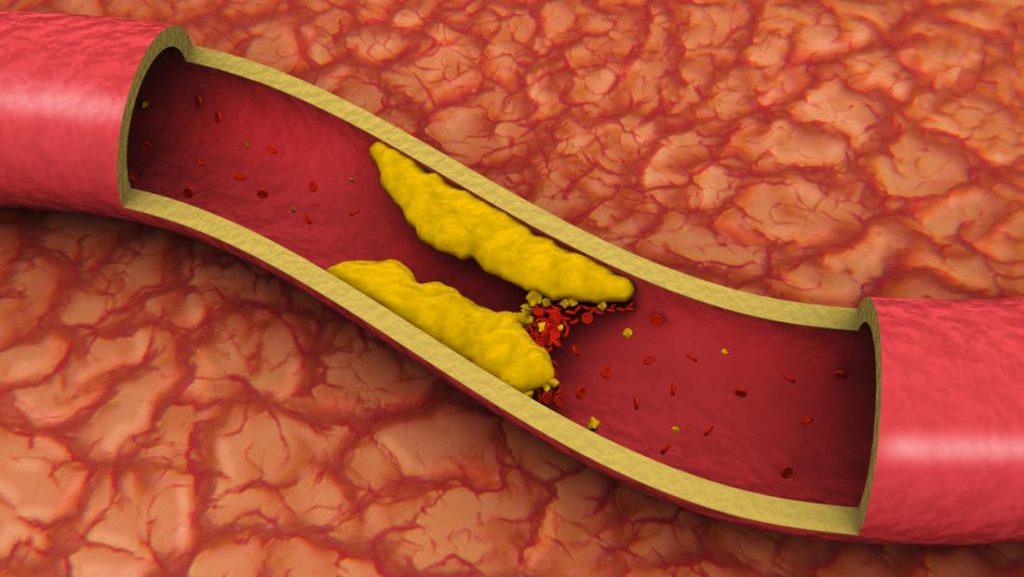
Out of all the studies that were reviewed, the researchers were able to identify 20 papers, with average sample sizes ranging from 28 to 64 and average study durations between 2 and 24 months. The findings of this study demonstrated that eating a vegetarian diet was linked to a reduction in LDL-C, or “bad” cholesterol, within six months. Additionally, it resulted in lower body weight and better HbA1c blood sugar readings. It revealed a lack of significance in the association between systolic blood pressure and plant-based diets.
This indicates that adding vegetarian eating habits into one’s diet may be advantageous for someone who has a high risk of developing cardiovascular disease.
According to this study, there is a direct link between a plant-based diet and a lower risk of developing cardiovascular and metabolic disease, said Litt. Therefore, trying a modified plant-based diet may be advantageous for people who are at higher cardiometabolic risk in the future.
Following a modified plant-based diet entails doing so once to twice per week to check on any changes in weight, HbA1c, or LDL cholesterol levels.
Diets high in vegetables may lower cholesterol.
The 1,878 participants in the study, who had cardiovascular disease (CVD) or were at high risk for developing it, were divided into 20 randomised controlled trials, with a mean age of 28 to 64 years. The number of participants varied depending on the study because not all the studies included the key measurements of LDL, weight, HbA1C, and systolic blood pressure. The majority of patients took medication to treat their cardiometabolic symptoms.
An average of six months was spent on each study. Nine included individuals who had at least two CVD risk factors, such as high blood pressure, high low-density lipoprotein (LDL) cholesterol, and diabetes, while four targeted persons with CVD. Seven focused on diabetes. Different vegan and vegetarian diets were consumed by the participants.
Measures of blood glucose, systolic blood pressure, or the amount of pressure in the arteries while the heart pumps blood, and LDL levels were included in the patient data (19 studies, 1,661 participants). Body weight was added as a supplementary metric.
In the end, the researchers discovered that following a vegetarian diet for an average of 6 months was associated with modest but significant drops in blood glucose and LDL levels.
They also noted that those with type 2 diabetes had the largest drops in blood sugar levels and those with a high risk of CVD got the greatest drops in LDL.
Additionally, participants (1,395 in 16 studies) lost an average of 3.4 kilogrammes during the course of the research, while blood pressure data (955 participants in 14 studies) showed no significant changes.
Vegetarian diets may be used in conjunction with medication-based therapy to prevent and cure a variety of cardiometabolic diseases, according to the study.
Why can eating vegetarianism lower the risk of CVD?
Dr. Hunnes was interviewed by specialists regarding the potential benefits of vegetarian diets for people with cardiovascular disease (CVD) or at high risk for developing it.
She pointed out that due to their higher intake of fruits, vegetables, grains, nuts, seeds, beans, and legumes as well as their lack of animal-based foods containing inflammatory saturated fats, vegetarian diets tend to be significantly richer in anti-inflammatory fibre and antioxidants.
This type of diet’s components tend to result in lower cholesterol levels, body weights, and inflammation. Together, [these variables] reduce [the risk of CVD],” she continued.
What are the research’s constraints?
According to the researchers, the results for cholesterol, blood pressure, and blood sugar may have been masked by patients’ usage of drugs to control these conditions. If so, they pointed out that vegetarian diets may have a greater impact on these measurements than was initially thought.
We also discussed the study’s shortcomings with Dr. John P. Higgins of McGovern Medical School at The University of Texas Health Science Centre at Houston (UTHealth), a sports cardiologist who was not involved in it.
The chance that a person’s commitment to a certain diet may decline with time, he said, limits the findings. Additionally, he emphasised that the Mediterranean diet and other diets known to promote heart health, such as vegetarian diets, were not contrasted in the study.
Dr. Zahir Rahman, a cardiologist at Staten Island University Hospital who was also unrelated to the study, was also the subject of a conversation with experts. He pointed out that the results are restricted because they are based on meta-analyses of studies with a small number of participants. However, he asserted that larger, higher-quality randomised studies would probably yield results that were comparable.
What kinds of vegetarian diets were mentioned in the paper?
The American Heart Association’s past president and Northwestern Medicine’s chief of cardiology, Dr. Clyde Yancy, who was not involved in the study, pointed out that it looked at a variety of vegetarian dietary patterns, including:
- The Ornish diet mostly consists of fruits, vegetables, whole grains, legumes, and soy, with only small amounts of nonfat dairy products,
- The lacto-ovo-vegetarian diet, which excludes meat but contains dairy and eggs,
- The lacto-vegetarian diet, which excludes eggs but include dairy products and is free of meat.
He pointed out that the findings highlighted the fact that there is no one universal vegetarian diet. He added a word of warning, saying that not all vegan options are low-fat and some may potentially contain high levels of fat.
The main message, according to Dr. Yancy, is the advantages of a diet rich in [diversity] in plant-based foods.
Resulting effects on cardiovascular health
Board-certified cardiologist Dr. Robert Pilchik of Manhattan Cardiology, who was not engaged in the study, stated:
This meta-analysis suggests that a vegetarian diet reduces LDL, [blood sugar], and body weight in synergy with best medical therapy. All of these are elements that raise the possibility of getting cardiovascular disease.
However, without going vegetarian, it might also be able to enhance cardiometabolic health, said Dr. Clancy.
Anyone may put the Life’s Essential 8 plan into practise right now, according to the American Heart Association. No one has to become a vegan or vegetarian, but everyone should be aware of the advantages of eating more plants,” he said in his conclusion.
REFERENCES:
- https://www.medicalnewstoday.com/articles/vegetarian-dietary-patterns-may-reduce-cardiovascular-disease-risk
- https://www.healthline.com/health-news/a-vegetarian-diet-may-help-improve-your-cholesterol-blood-sugar-levels-and-lead-to-weight-loss
- https://link.springer.com/article/10.1007/s00394-022-02942-8
For Cardiovascular disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_99