Sleeping well is incredibly important for lowering anxiety.
Chronic stress can make some mental diseases, such as anxiety and depression, more likely.
According to a new study, sleep and adaptive emotion regulation techniques both have a significant impact on lowering the risk of anxiety and depression in those who are under a lot of chronic stress.
This study made use of the COVID-19 pandemic, which caused a lot of chronic stress in the population. Regardless of the cause, managing chronic stress is important.

The COVID-19 epidemic created a rare circumstance in which many people went through a period of prolonged stress. Researchers want to know how long-term stress like this affects mental illness and what elements can help mental health.
The relationship between adaptive emotion regulation techniques, also known as positive coping mechanisms, and sleep quality was investigated in a study that was published in the journal Cortex.
Both elements are beneficial in lowering rates of anxiety and sadness, according to scientists. In contrast to their premise, they discovered that the quality of sleep did not significantly affect how well emotion management strategies worked.
What function does sleep quality have?
In this study, sleep and mental health data gathered from the spring of 2020 through the autumn of 2020’s COVID-19 pandemic were analysed secondarily.
The initial goal of the study was to determine whether adaptive emotion management techniques are related to greater mental health.
Long-term mental health is enhanced through thought processes known as adaptive cognitive emotion control techniques. A good illustration would be “positive reappraisal,” which is the process of looking for the positive aspects of an event or circumstance.
Second, scientists wanted to know if the efficiency of adaptive emotion management techniques was affected by the calibre of sleep. The COVID-19 pandemic was used as a naturally occurring and persistent stressor while they examined these factors.
Strategies for emotional management are crucial.
There were 1,600 adult participants in the study. The participants filled out online forms to submit information, including crucial demographic data. They also answered questions about general anxiety, despair, and sleep hygiene, as well as techniques for controlling emotions.
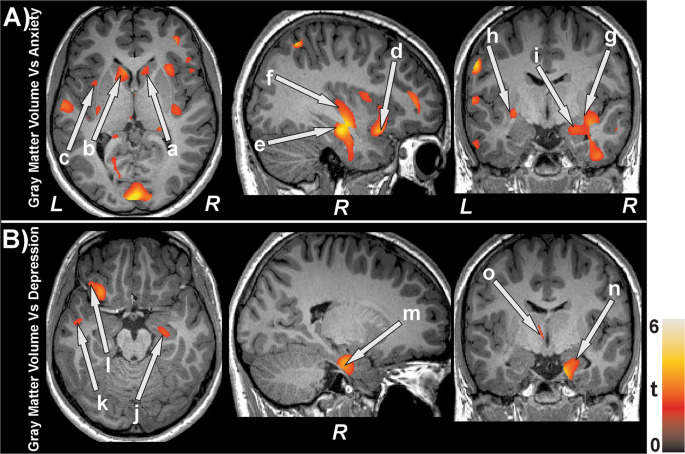
Based on data analysis, the researchers discovered that lower scores for anxiety and sadness were connected with greater usage of adaptive cognitive emotion control techniques.
Additionally, they discovered a link between claims of better sleep quality and lower anxiety and depressive disorder scores.
In terms of the connection between adaptive cognitive emotion regulation strategies and sleep quality, they discovered that persons who reported getting more restful sleep used these strategies more frequently.
Their final model, which took into account the quality of the sleep, revealed that employing adaptive cognitive emotion control techniques did not significantly predict the consequences of anxiety.
In other words, the quality of sleep did not seem to affect how successfully positive coping techniques reduced depression and anxiety. Regardless of the quality of sleep, the positive control techniques still demonstrated benefits for mental health.
Sullivan provided a nuanced explanation of these findings:
We did discover that using positive coping mechanisms more frequently was linked to fewer depressive and anxious symptoms. Additionally, fewer signs of anxiety and despair were linked to higher sleep quality. However, contrary to what we had anticipated, employing healthy coping mechanisms to lessen sadness and anxiety symptoms did not rely on getting enough sleep.
Findings are not as unexpected as they may appear
Dr. Lindsay Oberleitner, a licenced clinical psychologist and the education director of SimplePractice, who was not engaged in this study, offered her thoughts on the findings.
Contrary to expectations, she said, “cognitive emotion regulation strategies and sleep quality did not interact in their relationship to depression and anxiety.”
However, she added, this might not be as shocking as it initially appears to be.
“If we take a step back from the current study, this might not come as much of a surprise. We are aware that different people experience depression and anxiety in different ways due to complicated circumstances”. According to Dr. Lindsay Oberleitner, only a small part of emotion management techniques use adaptive cognitive strategies, and sleep is only one physical health factor that affects mental health.
Limitations of the study and future research
It is nonetheless important to be aware of this study’s limitations. Participants’ self-reporting, which is not always reliable, was used by researchers.
They observe that subjectively evaluated sleep quality is frequently poorer than what people report. They could only test sleep quality and adaptive cognitive emotion regulation technique once, thus they were unable to track changes that might have taken place over the course of the study.
Additionally, the authors had more data on depression than anxiety. The study lacked the capacity to detect any potential minor interaction effects.
They were unable to determine which cognitive emotion control method or combination was more effective due to the measurements they employed, as well as how these strategies worked together.
The majority of the white, educated female participants in the study were from the United States. Specific confounders could not be accounted for, and data was gathered online. All of these characteristics limit how broadly the study’s findings can be applied and point to the need for more diverse research in the future.
The COVID-19 pandemic presented a unique form of stress, therefore it is challenging to relate this study to other types of persistent stress and the ensuing mental health results, according to the study authors.
Since the COVID-19 pandemic was undoubtedly a particularly stressful circumstance, she said, “it would be beneficial to replicate these results in the context of other protracted stressful events.”
Additionally, she continued, “as we examined a variety of positive coping mechanisms together, it may be crucial in the future to see how particular mechanisms, like positive reappraisal (rethinking the circumstance in a positive light) and putting into perspective (i.e. considering the bigger picture), are related to both sleep quality and depressive and anxiety symptoms.”
How to deal with persistent stress?
Regardless of what causes it, managing stress requires action.For mental wellness, a trusted source is essential. This may entail making efforts to live a healthy lifestyle, asking friends for aid, and knowing when to seek the assistance of a mental health professional.
The World Health Organisation (WHO) adds that keeping a daily schedule and limiting time spent on social media can both help with stress management.
In Phoenix, Arizona, at Cora Health Solutions, Betsy Serrano, a board-certified psychiatric mental health nurse practitioner who was also not engaged in the latest study, provided the following advice for productive stress management:
“There are some straightforward exercises that can help reduce mild tension and anxiety. By releasing feel-good endorphins, physical activity releases stress-relieving hormones that help to calm the mind.” When feeling anxious, eating well, limiting caffeine intake, practicing yoga and meditation, as well some smartphone apps like Calm, are all quite beneficial. However, if your stress levels are so high that they’re interfering with your daily activities, you should think about seeking counselling and, if necessary, medication, according to mental health nurse practitioner Betsy Serrano.
REFERENCES:
- https://www.medicalnewstoday.com/articles/does-sleep-quality-really-play-a-key-role-in-reducing-anxiety-depression
- https://www.sleepfoundation.org/mental-health/anxiety-and-sleep
- https://www.everlywell.com/blog/sleep-and-stress/how-does-sleep-reduce-stress/
For Anxiety medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=31