New treatment may stop and potentially reverse some nerve damage in MS
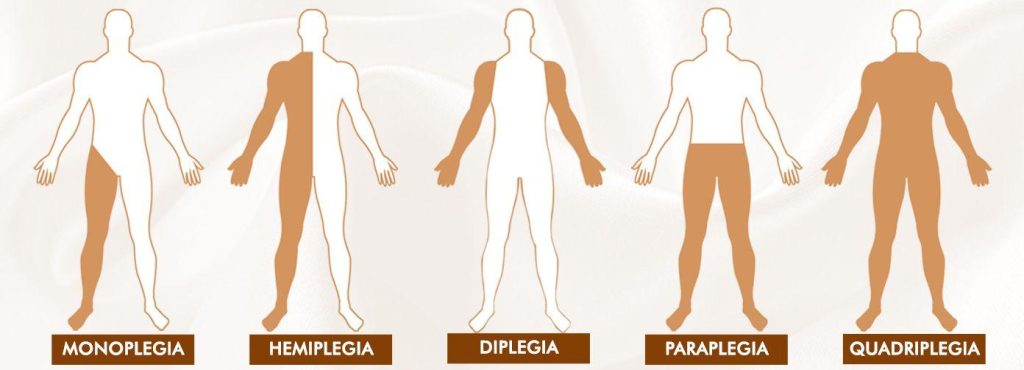
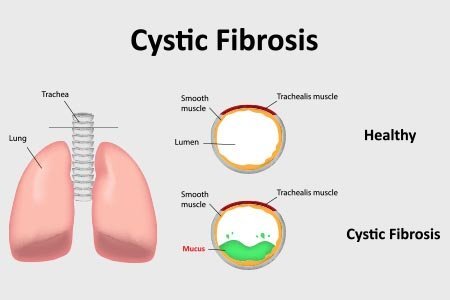
The neurological condition known as multiple sclerosis (MS) is a chronic illness that can cause paralysis, vision loss, and muscle weakness. It happens when the myelin sheath, which envelops and shields nerve cells, is attacked by the immune system. Current therapies seek to inhibit the immune system to stop additional nerve cell damage. A new study has produced a therapy that may be able to reverse the damage caused by multiple sclerosis and even help regenerate myelin.
The autoimmune disease known as multiple sclerosis (MS) causes the immune system to target and destroy the nerve cells’ myelin sheath. People in their 20s to 40s are the most common age range to experience it. The myelin sheath is attacked by immune cells, which results in inflammation and blocks the flow of nerve impulses throughout the body. This can cause neurological symptoms, such as fatigue, vertigo, bowel and bladder issues, muscle weakness, numbness, tingling, and pain, mobility issues, and vision loss.
Current therapies can alleviate symptoms, lessen the frequency and intensity of relapses, and slow the disease’s progression all while there is currently no known cure. Current treatments for MS work by targeting the immune system, which reduces the likelihood that the immune system will attack the protective myelin coating around nerves. Now, researchers have developed a treatment that can help regenerate myelin around nerve cells, potentially reversing the damage caused by MS. However, we also need to figure out how to fix the myelin that has already been harmed.
Restoring the protective sheath of nerve cells
Cells known as oligodendrocytes produce the myelin sheath that envelops and shields nerve cells. Myelin sheath damage cannot be repaired in an MS patient because these cells are lost in the disease. Regenerating myelin and activating oligodendrocytes have not always been successful in animal studies. A study on mice indicates that improving myelin production could be accomplished through an epigenetic strategy. A recently developed drug called PIPE-307 blocks the M1R receptor, allowing the oligodendrocyte precursor cells (OPCs) to differentiate into oligodendrocytes that can then form new myelin sheaths. The OPCs fail to differentiate into oligodendrocytes in people with MS. The researchers used this toxin from the venom of a green mamba snake to identify and locate this receptor protein on OPCs. Once the drug’s receptor had been identified and demonstrated to be able to block it, the researchers tested the drug’s effectiveness in vitro using isolated OPCs.
The medication caused the OPCs to develop into oligodendrocytes and start myelinating neighboring nerve axons because it blocked the M1R receptor more effectively than other medications. Additionally, because it could pass through the blood-brain barrier, it might be able to repair damaged brain nerve cells. After researching the biology of remyelination, we have developed a precise therapy to activate it, which is the first of a new class of MS therapies. Ten years ago, we found a way for the body to regenerate its myelin in response to the appropriate molecular signal, reversing the effects of MS.
Animal and phase 1 human trials show promise
Using slices of mouse brain tissue, the researchers conducted additional in vitro experiments and discovered that PIPE-307 enhanced the myelination of nerve cell axons. The drug was then given orally to mice (MOG-EAE mice) that had been genetically engineered to develop inflammatory demyelination as a model for multiple sclerosis. The mice not only displayed enhanced nerve cell myelination, but they also regained some of their lost functionality. This research, which used human tissue and animals, indicates that PIPE-307 has the potential to be used as a myelin repair treatment. Because PIPE-307 was well tolerated and had no negative effects in a phase 1 trial in healthy people, the researchers are moving on to a phase 2 trial to determine whether it is an effective treatment in people with MS. But to truly know whether this medication will be effective, we must see the outcomes of clinical trials involving MS patients.
Early progress could give hope to MS patients
With differing degrees of success, other medications, such as the first-generation antihistamine clemastine, have been studied as possible myelin repair therapies. The news release quoted Ari Green, MD, co-author of the paper and chief of the division of Neuroimmunology and Glial Biology in the UCSF Department of Neurology, as saying: “Clemastine is not a targeted drug, affecting several different pathways in the body.”. However, we quickly observed that its pharmacology with muscarinic receptors may lead to the development of more effective restorative treatments for MS patients.
Furthermore, their results imply that PIPE-307 is more successful in myelin restoration and M1R receptor blocking. It is still very early, though, and the recently started phase 2 trial will need to demonstrate that the medication is both safe and effective to take, with no serious side effects. As Astbury concluded, there is a critical need for efficient treatments for MS patients. Over 150,000 MS patients reside in the United States. K., and many of them lack access to any kind of care. We hope to see a cocktail of medications in the future that can stop immunological reactions, restore myelin, and shield nerves from additional harm. If additional trials prove fruitful, PIPE-307 might be included in that mix.
REFERENCES:
https://www.aol.com/treatment-may-stop-potentially-reverse-144117447.html
https://www.medicalnewstoday.com/articles/new-treatment-may-stop-potentially-reverse-nerve-damage-ms
Medications that have been suggested by doctors worldwide are available here
https://mygenericpharmacy.com/