Is Upper Respiratory tract, the most common infection?
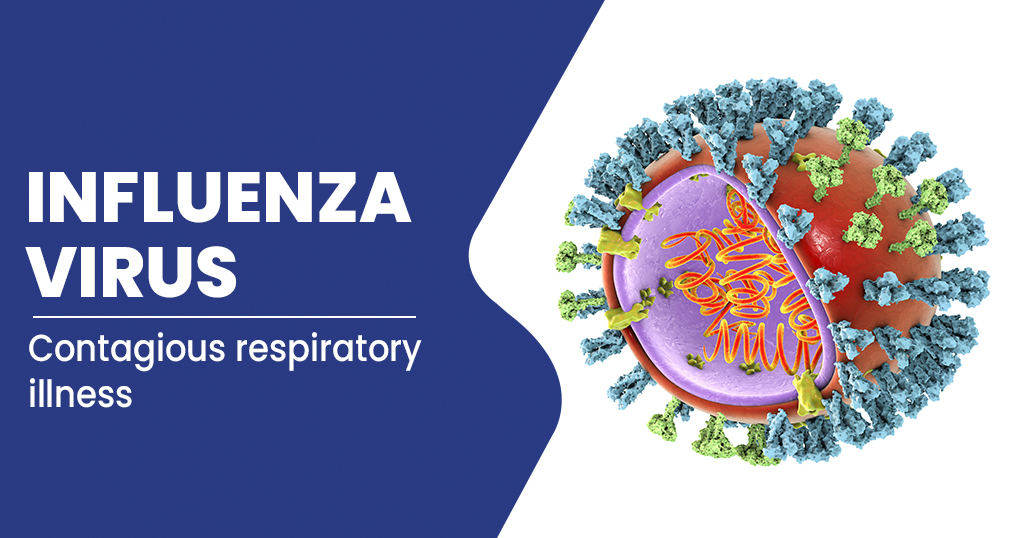
One of the most prevalent viral disorders, acute upper respiratory infections typically affect the nose and throat. They can persist up to 3 weeks and are frequently untreated.
Millions of people experience upper respiratory infections (URIs) each year. Although bacteria can also cause them, viruses typically cause them. The majority of URI sufferers recover within a few weeks, but some may experience complications that need medical attention.
What is Upper Respiratory Tract Infection?
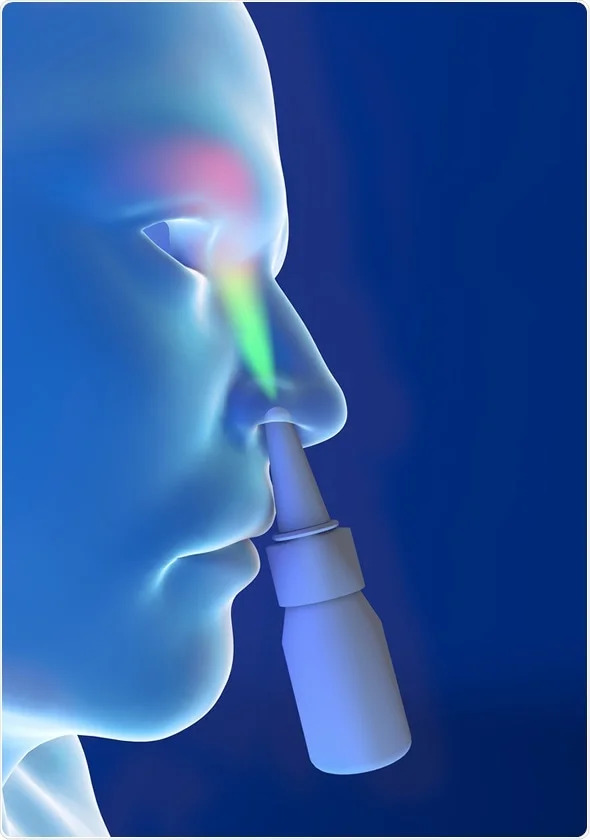
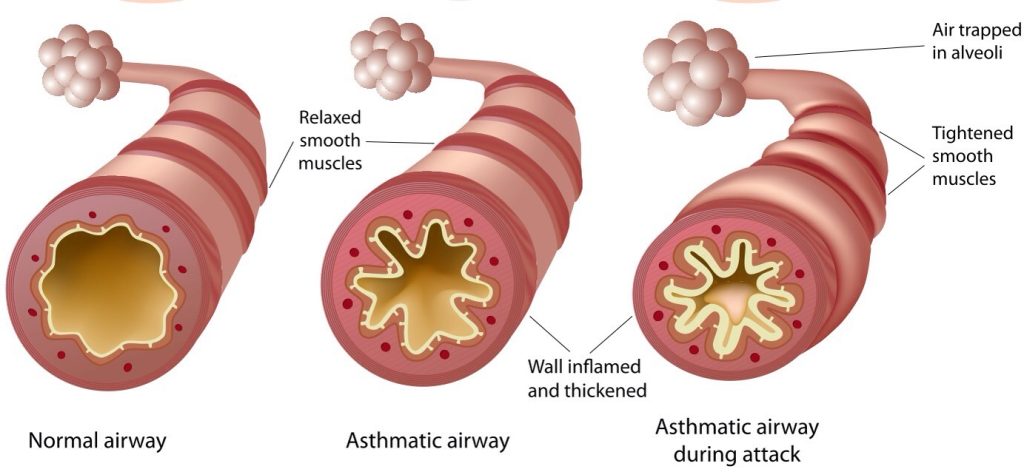
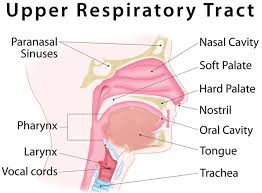
Nasal passageways and the throat are impacted by an upper respiratory infection (URI). Unless a person also has a persistent respiratory disease like Asthma, the therapy is typically straightforward. When a virus or bacteria enter the body, typically through the mouth or nose, a URI develops. Sneezing, coughing, or touching another person might spread the virus.
Adults often experience two to three URIs annually. Children, particularly young children, may experience more of these infections because of the immature state of their immune systems. Children are less likely than adults to wash their hands after sneezing or wipe their noses when necessary, thus children who spend a lot of time with other children may be more susceptible to these infections.
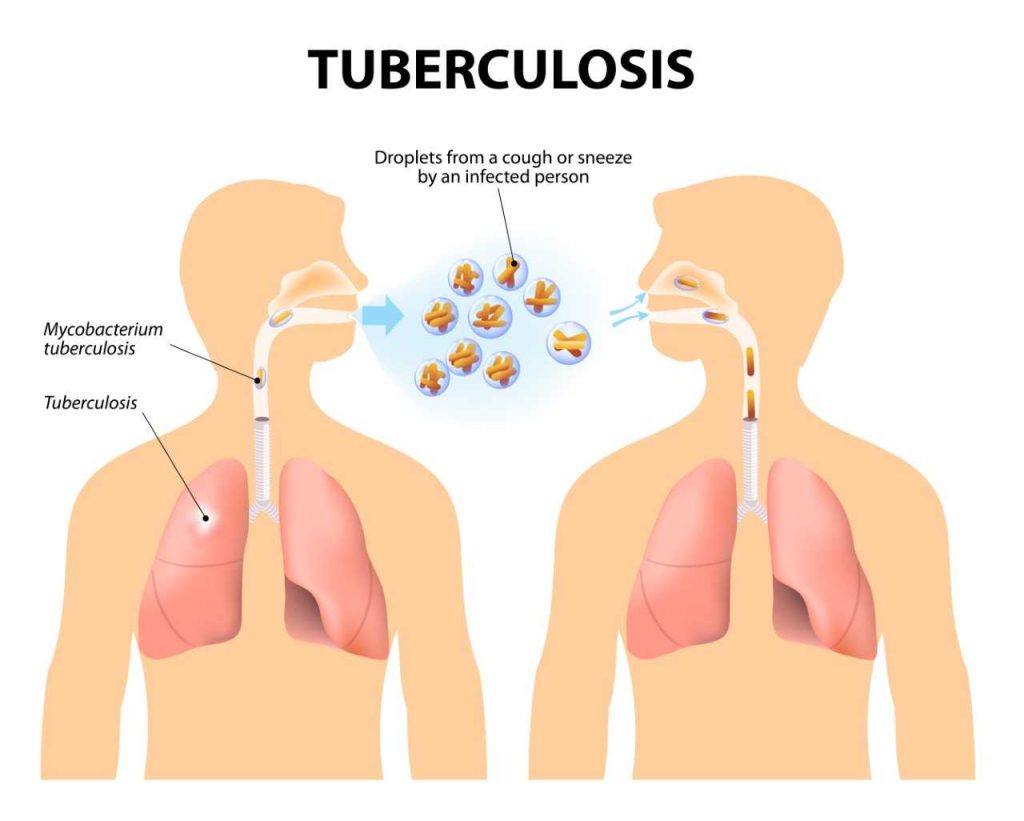
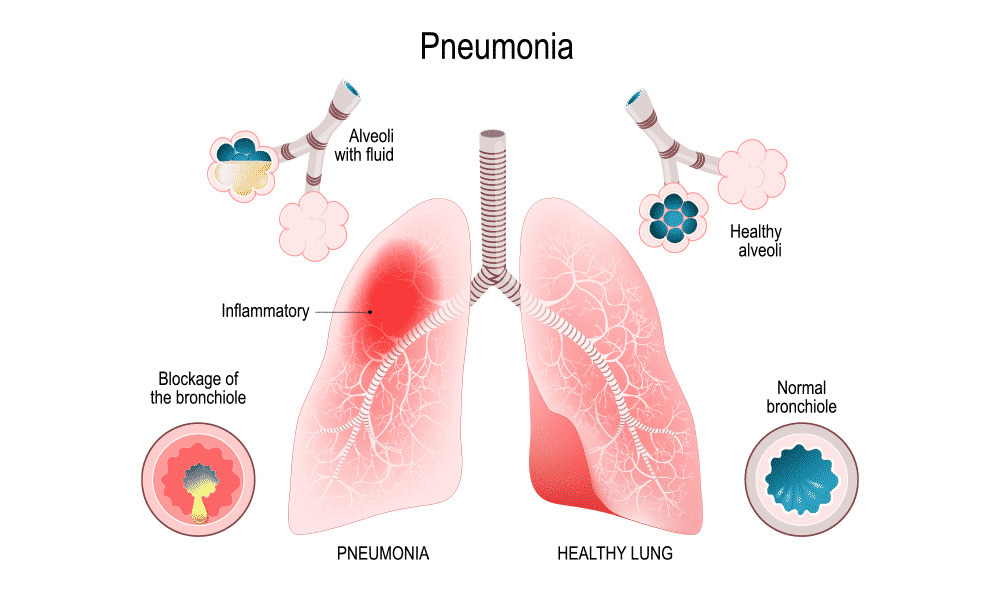
Homes, businesses, and other enclosed public spaces can pose a significant danger for the spread of URIs. A URI typically lasts 7–10 days, however it can occasionally last up to 3 weeks. These infections can occasionally worsen into more dangerous conditions like sinus infections or pneumonia.
Symptoms of upper Respiratory tract infection
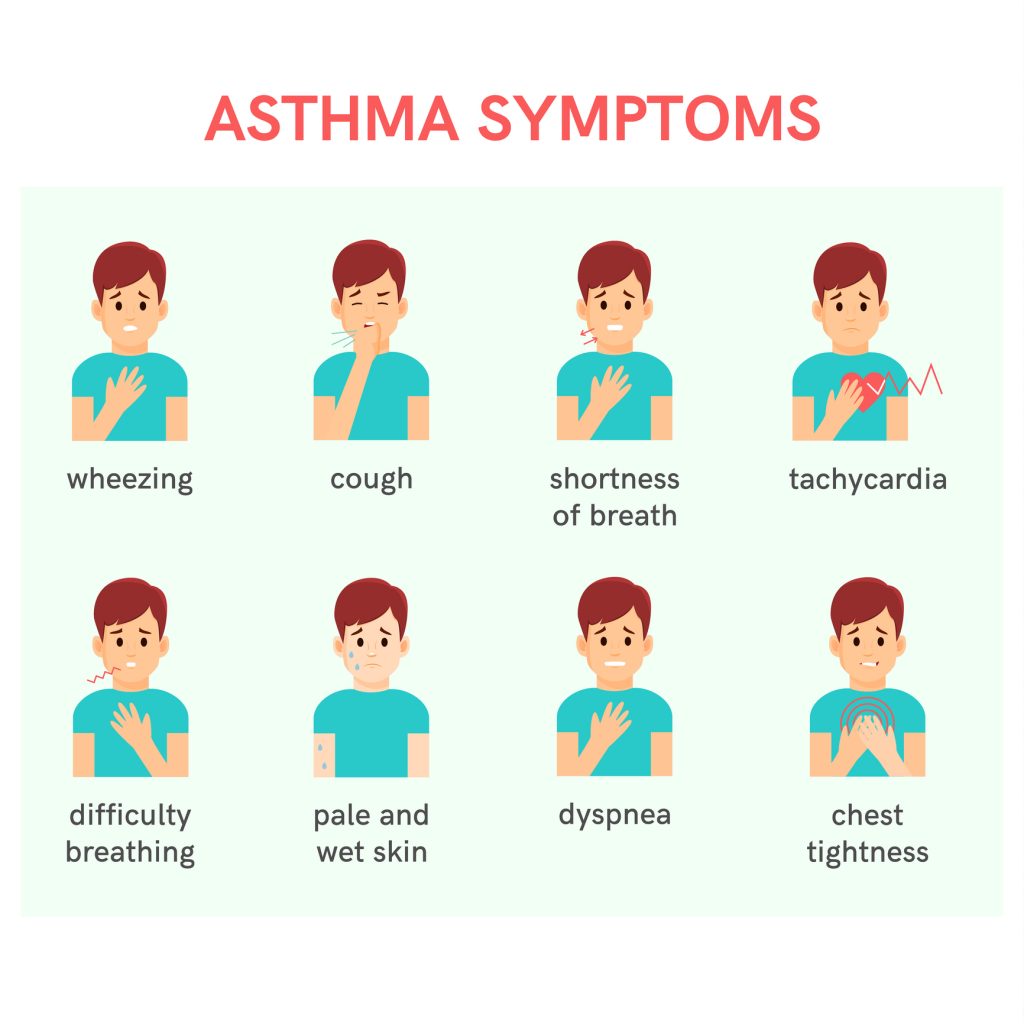
While various URIs can induce a variety of symptoms, the following are some of the more typical ones:
- coughing
- nasal congestion that is uncomfortable
- a little fever
- extra mucous
- nasal obstruction
- pressure or discomfort in the face
- running nose
- a painful or itchy throat
- sneezing
Additional signs can include:
- poor breath
- bodily pains
- a migraine
- Hyposmia, also known as a loss of scent
- scratchy eyes
Affected individuals often experience symptoms 1-3 days after coming into touch with an infected person, and they last for 7–10 days.
Types of upper Respiratory tract infection
There are various URI varieties, and medical professionals categorise them based on which area of the respiratory system they mostly impact. URI types include:
The common cold
A cold can be brought on by numerous viruses. Some signs could be:
- a runny or clogged nose
- an upset stomach
- headaches
- muscular pain
- sneeze and coughing
- alterations in flavour and odour
- the fever
- stress in the face and ears
After 10 to 14 days of at-home treatment, the symptoms often disappear.
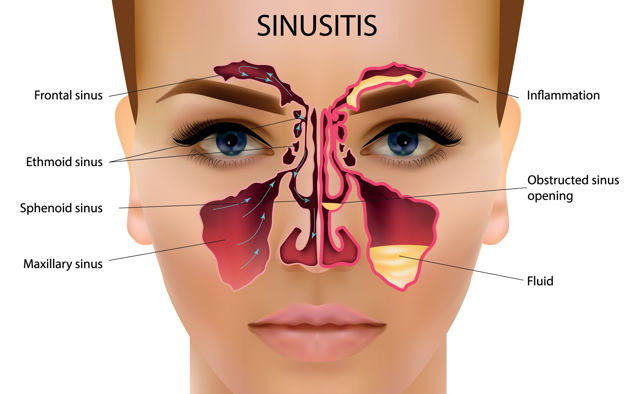
Sinusitis
Inflammation of the sinuses, or sinusitis, can result from an infection in another respiratory system organ. Due to difficulty draining, the inflammation may cause increased mucus production and closed sinuses.
Some signs of sinusitis include:
- discomfort in the forehead, cheeks, or eye area
- nasal discomfort and pressure
- nasal dripping
- a stuffy nose
- a diminished ability to smell
- the fever
- poor breath
If a person’s symptoms don’t go away after more than 10 days, they should see a doctor.
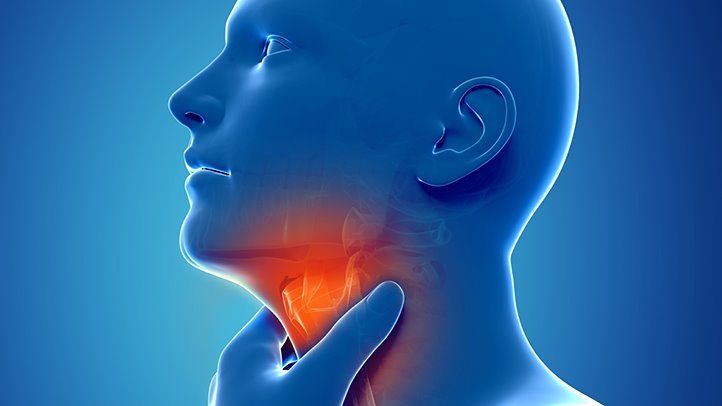
Laryngitis
This is inflammation of the larynx, which is another name for the vocal chords.
Some typical signs include:
- a voice loss or hoarseness
- a persistent cough and throat irritation
- an upset stomach
Typically, the symptoms last 7 to 10 days.
Pharyngitis
Inflammation of the mucous membranes lining the pharynx, or back of the throat, is known as pharyngitis. It frequently happens with URIs.
Symptoms of pharyngitis include the following:
- an itchy or painful throat
- inflammation
- fever
- headache
- having trouble swallowing
The throat’s walls may have ulcers, a doctor may discover.
Additional symptoms
The following situations require medical intervention for the individual:
- an extreme fever
- severely distressed breathing
- having trouble swallowing
Who is at risk for upper respiratory infection infection?
The most frequent reason for healthcare visits in the US is the common cold. Aerosol droplets and direct hand-to-hand contact are two ways that URIs are transferred from one person to another. The risk increases:
- When a sick person sneezes or coughs without covering their mouth and nose, virus-carrying droplets are released into the atmosphere.
- when people are crammed together or in an enclosed space, such as at daycare centres, hospitals, and other establishments.
- if you suffer from an illness like asthma or allergic rhinitis.
- if you have a compromised immune system, such as cystic fibrosis or HIV in smokers.
- when people use corticosteroids, such as prednisone.
REFERENCES:
- https://www.healthline.com/health/acute-upper-respiratory-infection
- https://www.medicalnewstoday.com/articles/323886
- https://my.clevelandclinic.org/health/articles/4022-upper-respiratory-infection
- https://www.medicinenet.com/upper_respiratory_infection/article.htm
For more details, kindly visit below.