What are the foods that keeps healthy and supple skin?
Numerous foods contain antioxidants, vitamins, and minerals that can assist to improve the health of your skin.
Studies reveal that plant-based diets can actually assist enhance skin elasticity and hydration since they are particularly rich in nutrients that support the skin, such as vegetables, fruits, nuts, seeds, and beans. They might possibly aid in lessening wrinkle visibility.

There isn’t a special superfood for healthy skin. Instead, what matters is your entire nutritional pattern. The greatest method to encourage healthy skin is to consume a diet high in plants and oily fish in moderation.
It is becoming more and more obvious that what you eat has a substantial impact on the health and ageing of your skin as scientists understand more about diet and the body.
What makes food good for your skin?
Vitamin C, vitamin E, beta-carotene, and polyphenols are a few elements found in plant-based meals that serve as antioxidants. These antioxidants maintain the structural support of the skin, lessen inflammation, and protect against oxidation. They also have a lot of beans, fruits, vegetables, coffee, and tea.
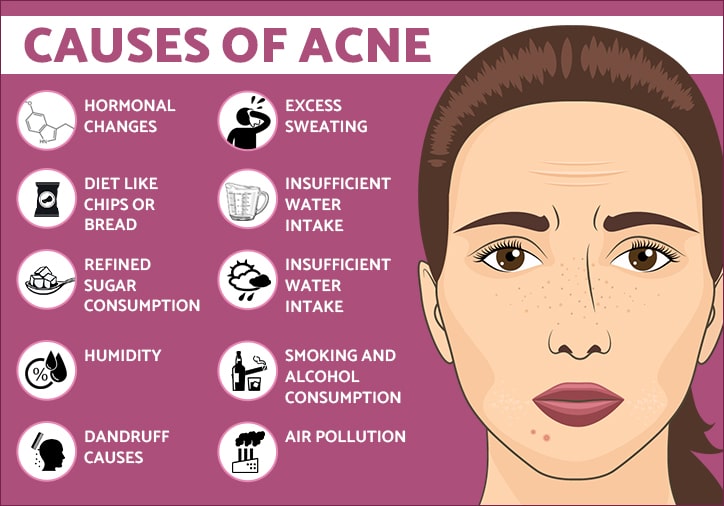
Polyunsaturated fats, found in foods like nuts, seeds, and fatty seafood, are essential for maintaining good skin. These fats, which comprise omega-3 and omega-6 fatty acids, may lessen inflammation, which could aid in the treatment of skin diseases like atopic dermatitis, psoriasis, and acne.
According to one study, eating a diet high in plant-based foods is linked to less face wrinkles, whereas eating a diet high in red meat and snack foods is linked to more facial wrinkles. Therefore, it makes sense to consume less ultra-processed foods and more plant-based foods.
The best foods and beverages for your skin
Fatty fish
Salmon, mackerel, and herring are all good sources of fat for maintaining healthy skin. They are abundant in omega-3 fatty acids, which are crucial for preserving the health of the skin.
Omega-3 fatty acids are essential for maintaining healthy, thick, supple skin. In actuality, a lack of omega-3 fatty acids can lead to dry skin. Since inflammation can result in redness and acne, fish’s omega-3 fats help to alleviate it. They may even lessen your skin’s sensitivity to UV rays from the sun.
According to some research, fish oil supplements may aid in the treatment of inflammatory and autoimmune skin disorders like lupus and psoriasis.
Avocados
Healthy fats are abundant in avocados. These fats help your body in various ways, including with skin health. It’s crucial to consume enough of these fats to maintain skin supple and hydrated. A high consumption of total fat, specifically the good fats found in avocados, was linked to more elastic, springy skin, according to a study involving over 700 women.
Additionally, preliminary research suggests that avocados contain substances that could help shield your skin from solar damage. Wrinkles and other ageing symptoms can be brought on by UV damage to your skin.
Vitamin E, a vital antioxidant that aids in preventing oxidative damage to your skin, is another crucial nutrient that can be found in abundance in avocados. The majority of Americans do not consume enough vitamin E.
Walnuts
Walnuts are a great food for healthy skin because of a variety of factors. They are a good source of vital fatty acids, which your body needs but cannot produce on its own.
In fact, they contain more omega-3 and omega-6 fatty acids than the majority of other nuts. An excessive intake of omega-6 fatty acids may encourage inflammation, including skin diseases like psoriasis.
Omega-3 fatty acids, on the other hand, reduce inflammation throughout your body, especially in your skin. Omega-3 fatty acid sources are few compared to omega-6 fatty acid sources in the Western diet.
Walnuts have a healthy balance of these fatty acids, which may assist them combat any potential inflammatory reactions to too much omega-6.
Sunflower seeds
Nutrients that are excellent for the skin can be found in abundance in nuts and seeds. Sunflower seeds are a great illustration.
Sunflower seeds include 5.5 grammes of protein, 49% of the daily value (DV) for vitamin E, 41% of the DV for selenium, and 14% of the DV for zinc in one ounce (28 grammes).
The sweet potato
A nutrient called beta carotene is present in plants. It performs as a provitamin A, which means your body can change it into vitamin A. Oranges and vegetables including spinach, carrots, and sweet potatoes contain beta carotene.
One half-cup (100 grammes) serving of baked sweet potatoes contains enough beta carotene to supply more than six times the DV for vitamin A, making them a great source. By serving as a natural sunblock, carotenoids like beta carotene aid in maintaining the health of your skin.
This antioxidant is absorbed into your skin after consumption and aids in shielding your skin’s cells from UV radiation. This may lessen the risk of skin cancer, cell death, and wrinkled, dry skin.
Yellow or red bell peppers
Bell peppers are a great source of beta carotene, which your body turns into vitamin A, just like sweet potatoes are. The amount of vitamin A in one cup (149 grammes) of finely chopped red bell pepper is equivalent to 156% of the DV.
Additionally, they are among the greatest sources of vitamin C. The production of the collagen protein, which maintains skin strong and firm, depends on this vitamin.
149 gram or one cup of bell peppers contain an astounding 211% of the daily value (DV) for vitamin C. Eating a lot of vitamin C was associated to a lower chance of developing wrinkles and dry skin as people age in a significant observational research involving women.
Broccoli
Zinc, vitamin A, and vitamin C are just a few of the vitamins and minerals abundant in broccoli that are crucial for healthy skin.
Additionally, it has lutein, a pigment that functions similarly to beta carotene. Lutein aids in preventing oxidative skin damage, which can lead to dryness and wrinkles in the skin. But sulforaphane, a unique substance found in broccoli florets, also packs a powerful potential punch. Even some varieties of skin cancer may be resistant to it’s effects.
Sulforaphane is also an effective solar damage preventative. It functions in two ways: by scavenging dangerous free radicals and activating additional defence mechanisms within your body.
Tomatoes
The main carotenoids, including lycopene, and vitamin C are all present in tomatoes. It has been demonstrated that beta carotene, lutein, and lycopene can shield your skin from UV damage. They might also aid in avoiding wrinkles.
Tomatoes are a great meal for preserving good skin since they are high in carotenoids. Think about combining foods like tomatoes that are high in carotenes with a source of fat, such cheese or olive oil. Your body absorbs more carotenoids if you are fat.
Soy
Isoflavones, a class of plant compounds found in soy, have the ability to either imitate or prevent the effects of oestrogen in your body. Your skin may benefit from isoflavones, among other regions of your body.
In a small research of middle-aged women, it was discovered that consuming soy isoflavones daily for 8–12 weeks decreased fine lines and increased skin suppleness. Soy may benefit postmenopausal women with skin dryness issues and may boost collagen production, which keeps skin strong and supple.
These isoflavones not only help to shield your body’s internal cells from harm but also your skin from UV radiation, which may lower your risk of developing some types of skin cancer.
Dark chocolate
Here’s one more justification, in case you needed it: On your skin, cocoa has some pretty amazing properties. Participants in one study reported fuller, more moisturised skin after taking an antioxidant-rich cocoa powder daily for 6–12 weeks.
Additionally, their skin had greater blood flow, which carries more nutrients to the skin, and was less scratchy and scaly, as well as less vulnerable to sunburn.
Another study discovered that consuming 20 grammes of high-antioxidant dark chocolate daily could increase your skin’s ability to withstand more than twice as much UV radiation before burning.
Similar outcomes, including changes in the appearance of wrinkles, have been seen in several other investigations. Keep in mind, nevertheless, that at least one study did not discover any appreciable effects.
Green tea
Your skin may benefit from green tea’s ability to prevent ageing and damage. Catechins, potent substances included in green tea, have been shown to benefit skin health in a number of ways. Green tea, like a number of other foods high in antioxidants, can help shield your skin from UV damage.
One 12-week study involving 60 women discovered that drinking green tea on a regular basis could cut sunburn redness by up to 25%. Additionally, green tea enhanced their skin’s elasticity, thickness, roughness, and moisture content.
Water
Without mentioning the advantages of staying well hydrated, no list regarding skin health would be complete.
A wise decision is to constantly drink lots of water. Since water makes up up to 64% of skin cells, it significantly affects the health and appearance of your skin. While a severe dehydration can cause dry skin, several research suggest that drinking enough water has favourable effects on typical skin physiology.
Above list does not contain all of the food that can help in improving skin health.
Your skin’s health can be dramatically impacted by what you consume. Make sure you’re receiving the necessary nutrients to keep your skin protected. The foods on this list are excellent choices for maintaining the strength, radiance, and health of your skin.
REFERENCES:
- https://www.webmd.com/beauty/ss/slideshow-skin-foods?
- https://www.healthline.com/nutrition/12-foods-for-healthy-skin
- https://www.goodrx.com/well-being/diet-nutrition/foods-good-for-skin
For more details, kindly visit below.