Long-term melatonin use linked to 90% greater heart failure risk.
Approximately 16% of people worldwide suffer from insomnia. A person can enhance the quality of their sleep in a variety of ways, including by taking melatonin supplements. Previous research indicates that using melatonin supplements may pose certain risks. According to a recent study, taking melatonin supplements over an extended period of time may increase the risk of heart failure. According to research, 16% of people worldwide suffer from insomnia, which is the inability to fall or stay asleep. A person can enhance the quality of their sleep in a variety of ways. Among them are behavioral adjustments like maintaining proper sleep hygiene, exercising during the day, and avoiding certain foods right before bed. Other individuals who have trouble falling asleep may choose to use medical interventions, such as prescription drugs or over-the-counter remedies like melatonin supplements, a hormone that the body produces naturally and is crucial.
12-month or longer melatonin use linked to 90% greater heart failure risk
Researchers examined medical records from TriNetX for nearly 131,000 adults who had been diagnosed with insomnia, with an average age of roughly 56. Approximately 65,000 study participants reported taking melatonin for at least a year after receiving a prescription for it at least once. According to the study’s findings, individuals who took melatonin for longer than a year had a 90% higher risk of heart failure over five years than those who did not. Additionally, participants had an 82% higher risk of heart failure if they had filled at least two melatonin prescriptions at least ninety days apart. Furthermore, during the five-year follow-up period, researchers found that melatonin users were roughly 3.5 times more likely to be hospitalized for heart failure and twice as likely to die from any cause.
Melatonin supplements are widely thought of as a safe and ‘natural’ option to support better sleep, so it was striking to see such consistent and significant increases in serious health outcomes, even after balancing for many other risk factors, Ekenedilichukwu Nnadi, and lead author of the study, said in a press release. Worse insomnia, depression/anxiety or the use of other sleep-enhancing medicines might be linked to both melatonin use and heart risk. Also, while the association we found raises safety concerns about the widely used supplement, our study cannot prove a direct cause-and-effect relationship. This means more research is needed to test melatonin’s safety for the heart, Nnadi explained
Unexpected findings on melatonin and heart health are noteworthy
Melatonin is widely regarded by both the public and many in the medical community as a safe, ‘natural’ sleep aid, so it was striking to see a potential link to serious health issues like heart failure, Mody explained. While this study shows an association and not a direct cause-and-effect relationship, the consistency and significance of the increased risks are noteworthy. It’s particularly unexpected given that some previous research has suggested potential cardiovascular benefits of melatonin, such as its antioxidant properties.
This new study challenges the conventional wisdom regarding long-term melatonin use for chronic insomnia, for which it is not an indicated treatment in the United States, she continued. According to Mody, these findings suggest a re-evaluation of how we counsel patients about sleep aids and underscore the importance of discussing long-term supplement use. My concern is that insomnia may actually be masking signs and symptoms of early heart failure in some of these cases, so this research also highlights the importance of ruling out different causes of insomnia, particularly since the treatment market for insomnia aids is not strongly regulated.
Further research is needed to confirm the findings
According to Mody, the research’s next steps should concentrate on a number of crucial areas to elucidate the results and their consequences for patient care, such as causality and confirmation. She explained, “First and foremost, more research is needed to confirm these findings and to determine if there is a direct cause-and-effect relationship between long-term melatonin use and heart failure. The best way to determine whether melatonin is safe for the heart would be to conduct randomized controlled trials. Research will need to investigate the biological mechanism by which long-term melatonin use might increase the risk of heart failure if a causal link is established, Mody continued. Given that melatonin has been shown to have protective effects on the cardiovascular system, this would be a major change
How can I improve my sleep without taking melatonin?
Melatonin is available in a variety of formulations, including high and low doses, as well as slow and immediate release, none of which are FDA regulated, according to Ni’s initial response to the study. Therefore, there are worries that the levels of melatonin drugs and supplements may differ significantly. It is difficult to determine whether a particular amount or kind of melatonin is linked to an increase in heart failure.
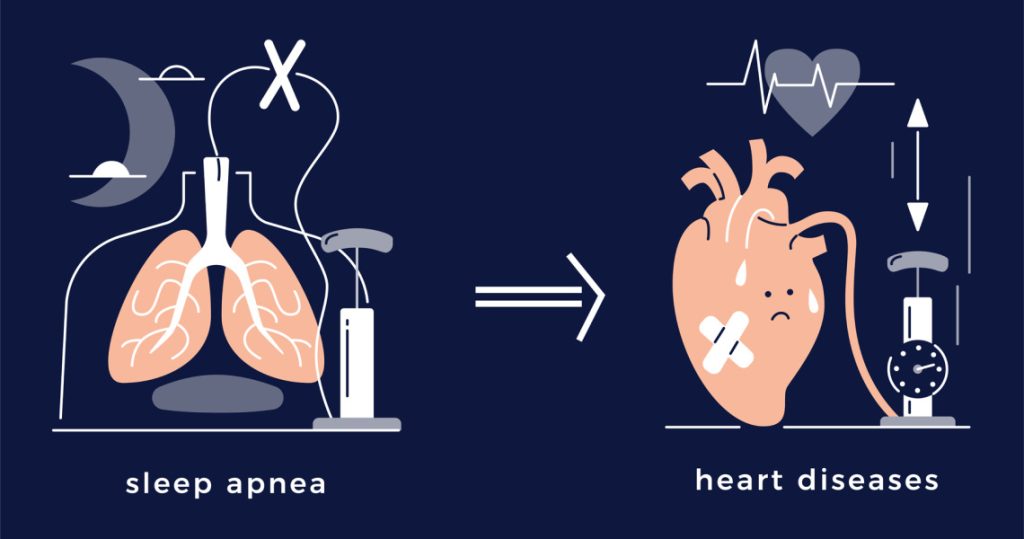
However, considering that melatonin is not subject to FDA regulation, the study is undoubtedly concerning, he said. Ni strongly suggests that people who may be taking melatonin think about other ways to enhance the quality of their sleep. He clarified, for instance, that a lot of people have sleep apnea but are unaware of it and mistakenly believe that they just need to take a sleep aid to help them sleep. Given that sleep apnea is linked to an increased risk of heart disease, melatonin users in the study may have sleep issues.
I should also mention that melatonin and high dosages seem to have a paradoxical effect on sleep; that is, taking too much melatonin may actually make it difficult for you to fall asleep. I typically advise my patients to take no more than 1 to 3 mg of melatonin per night. Additionally, I tell my patients that because the melatonin hormone’s effect on sleepiness is gradual, it usually needs to be taken at least an hour or two before attempting to fall asleep.
https://mygenericpharmacy.com/category/disease/sleep-disorder