Hypertension: Even a single drink of alcohol can add to it.
Heart attacks and other ill health outcomes are made more likely by high blood pressure. The risk of high blood pressure can be affected by a variety of variables, including lifestyle decisions.
Researchers are still trying to fully comprehend how various lifestyle decisions affect blood pressure levels.
According to data from a recent study, drinking alcohol raises systolic blood pressure, even at moderate doses of alcohol consumption.

A crucial health indicator is blood pressure. Reduced risk of negative health effects can be achieved by maintaining optimal blood pressure levels. Hypertension, often known as high blood pressure, can be caused by a variety of circumstances. Researchers are still working to fully comprehend the effects of these risk variables, though.
The effect that drinking alcohol has on blood pressure is one topic of interest. Alcohol consumption is widespread, even at tiny doses. It’s consumption can raise blood pressure, albeit it may only be in tiny amounts.
Alcohol consumption, even as little as one drink per day, was linked to higher blood pressure, according to a study published in the journal Hypertension.
High blood pressure effects and risk factors
The force of blood pushing against the body’s arteries is measured by blood pressure. Systolic and diastolic blood pressure measurements reflect the contraction and relaxation of the heart, respectively.
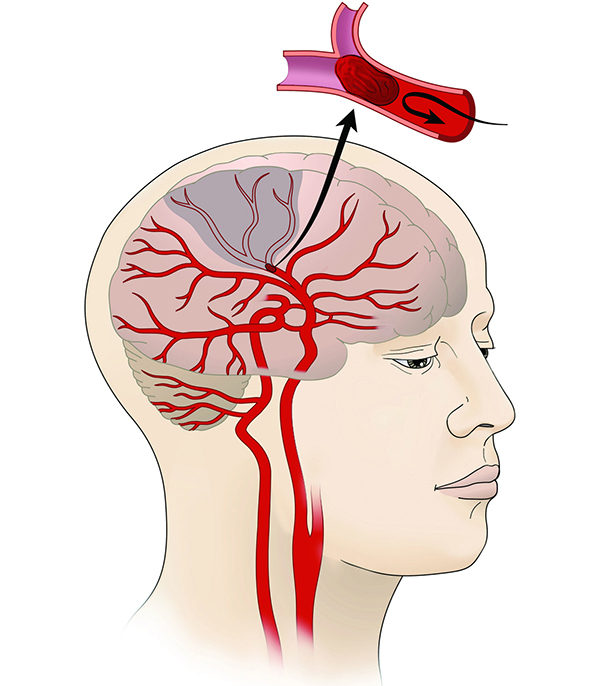
When blood pressure rises too high, there is a higher chance that the body will sustain harm. For instance, high blood pressure can raise the risk of heart failure and heart attack.
Smoking, consuming a diet heavy in sodium, and having little physical activity are risk factors for high blood pressure. Consuming alcohol can elevate risk. The Centres for Disease Control and Prevention (CDC) and other organisations currently advocate for limiting alcohol consumption to one drink per day for women and two drinks per day for men.
Current recommendations were further explained by Dr. Cheng-Han Chen, an interventional cardiologist and the medical director of the Structural Heart Programme at MemorialCare Saddleback Medical Centre in Laguna Hills, California.
We have long known that consuming alcohol in moderate to high doses will increase blood pressure. This has a lot to do with cardiovascular health because increased blood pressure, also known as hypertension, is a significant risk factor for heart attacks and strokes, among other cardiovascular disorders. We have advised people to limit their alcohol consumption to a “moderate” level (2 drinks per day for men and 1 drink per day for women).
Alcohol’s effects on blood pressure
How much alcohol affects the risk of high blood pressure is one topic that needs more research. To comprehend how various alcohol consumption levels affected blood pressure levels, researchers for the current paper wanted to know. Does alcohol consumption, for instance, affect risk even at modest doses?
This study involved the dose-response meta-analysis of seven various non-experimental cohort studies. To gather a massive amount of data, researchers examined the data from over 19,500 participants. United States, Japanese, and South Korean subjects were involved in the studies.
Almost five years were spent on follow-up on average. To ensure that only participants without a prior history of cardiovascular illness were included in studies, strict eligibility requirements had to be met by each one.
They discovered that, on average, drinking 12 grammes of alcohol per day resulted in a 1.25 mmHg rise in systolic blood pressure. Twelve grammes of alcohol is even less than the fourteen grammes of alcohol in a regular American drink.
Higher alcohol intakes were linked to a more pronounced rise in systolic blood pressure, with 48 grams per day of alcohol being linked to an average rise of 4.9 mmHg.
Author of the study and adjunct professor in the epidemiology division at Boston University’s School of Public Health, Dr. Marco Vinceti, from the University of Modena and Reggio Emilia in Italy:
The overall (or “public health”) message for the relationship between alcohol consumption and blood pressure that emerged from our dose-response meta-analysis is “the lower the better, and no consumption even better,” as we were unable to find any evidence that even very small amounts of alcohol consumption might be beneficial for people’s health.
Research limits and future directions
There are significant limitations to the data in this study. First, there wasn’t a lot of research accessible for analysis. The association between age, blood pressure, and alcohol consumption was not able to be thoroughly investigated. Misclassifications were a possibility, and some individuals’ levels of alcohol use likely changed over the follow-up period. Additionally, the study did not investigate the effects of various types of alcohol on blood pressure. Some data depended on self-reporting; further data could use more representative samples.
In the studies that met the eligibility requirements, there was a special risk for bias, and there is still a possibility for residual confounding. There are numerous chances to build on the research, including learning more about how alcohol consumption affects women’s blood pressure.
Dr. Vinceti identified the following issues as needing more study:
“Our systematic review and dose-response meta-analysis concentrated on a continuous endpoint, changes in blood pressure over time, but it did not look at ‘hard outcomes’ like hypertension (as a dichotomous outcome), stroke (for which high blood pressure is an established and strong risk factor), coronary heart disease, and ultimately overall CVD risk. Therefore, to paint a complete picture of the consequences of alcohol use on the cardiovascular system, our study must be supplemented with such additional (and updated) assessments.”
The results of this study may alter recommendations for alcohol consumption, albeit it will probably take time and additional study. On this subject, Dr. Chen made the following assumptions:
“For a very long time, the general opinion was that drinking in moderation might be considered safe.” This study supports other recent results that indicate that consuming alcohol at any level is not beneficial for the heart. As a result, I anticipate that in the future, medical advice about alcohol intake will change.
REFERENCES:
- https://www.medicalnewstoday.com/articles/hypertension-1-alcoholic-drink-a-day-higher-blood-pressure
- https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/limiting-alcohol-to-manage-high-blood-pressure
- https://www.cbsnews.com/news/alcoholic-drink-linked-to-higher-blood-pressure/
For High blood pressure medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=8