People with blocked arteries may get stroke during exercise
Exercise may cause a stroke in patients with severely blocked arteries, according to research. The study, according to experts, is intriguing but they point out that it is based on a computer model.
They also point out that the majority of people who don’t have clogged arteries still benefit from exercise.
It turns out there is a purpose for the recommendations to visit a doctor before beginning new workout programs that are typically included with them.

In people with blocked or restricted carotid arteries, exercise may increase the risk of stroke. This is according to a recent study published in Physics of Fluids.
Even so, carotid stenosis, which is another name for this ailment, only affects about 3% of the general population.
According to the study, those who have moderate to severe artery blockage should exercise with caution. But the majority of people gain from regular exercise, which is advised for heart health.
The researchers also concluded that exercise is still helpful for preserving healthy blood flow in those who are in good health. Also, in those whose arteries are only mildly clogged.
Exercise increases heart rate and can increase stroke risk.
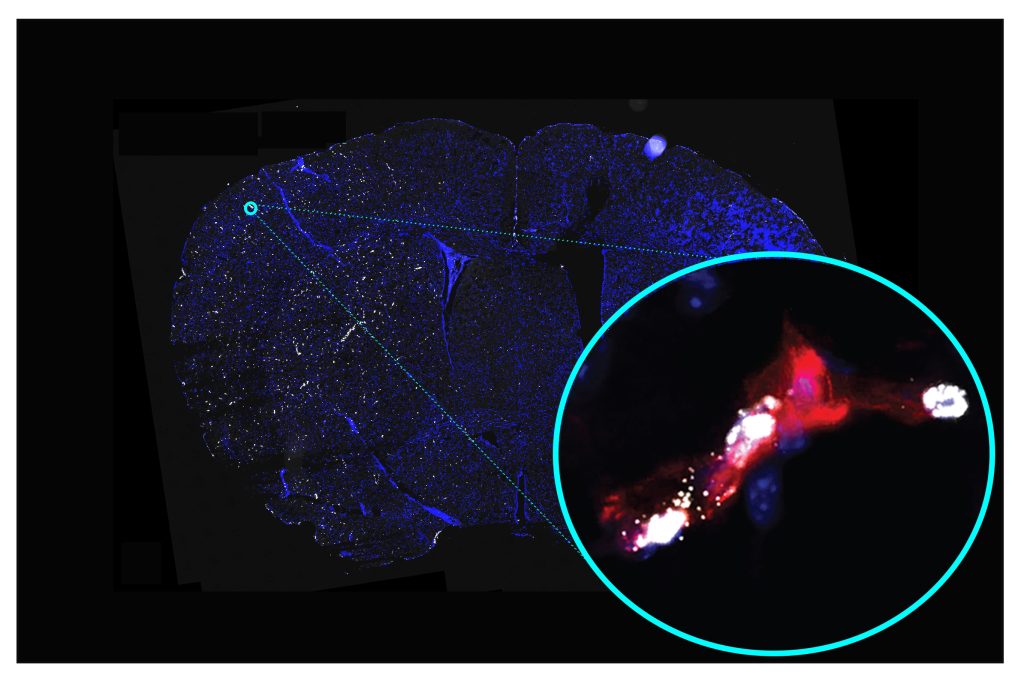
Researchers examined the relationship between exercise-induced heart rates and resting heart rates for the study.
They stimulated blood flow in carotid arteries in the following stages of stenosis using a computational model:
- without obstruction
- a little 30% obstruction
- having a medium 50% obstruction
According to the research, exercise increased stress in the arteries’ obstructed region in persons with mild blockages. This increased the risk of stenosis rupture.
A stroke that is ischemic could result from this blockage once it enters the brain. But exercise helped the stimulated carotid in people with no stenosis or modest blockage.
Dr. Somnath Roy, Ph.D., an associate professor of mechanical engineering at the Indian Institute of Technology Kharagpur, India, is the study’s lead author. “Intense exercise shows adverse effects on patients with moderate or higher stenosis levels,” he stated in a statement.
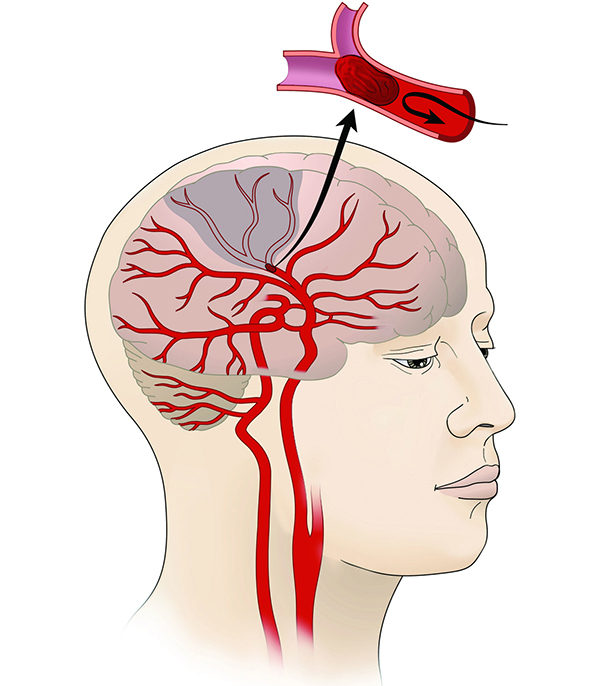
It significantly raises the shear stress at the stenosis zone, raising the risk of the stenosis rupturing. The blood from the ruptured plaque may then reach the brain’s blood supply and result in an ischemic stroke.
The study team also suggested that a high heart rate would make it more likely for another stenosis to emerge.
How dangerous are blocked carotid arteries?
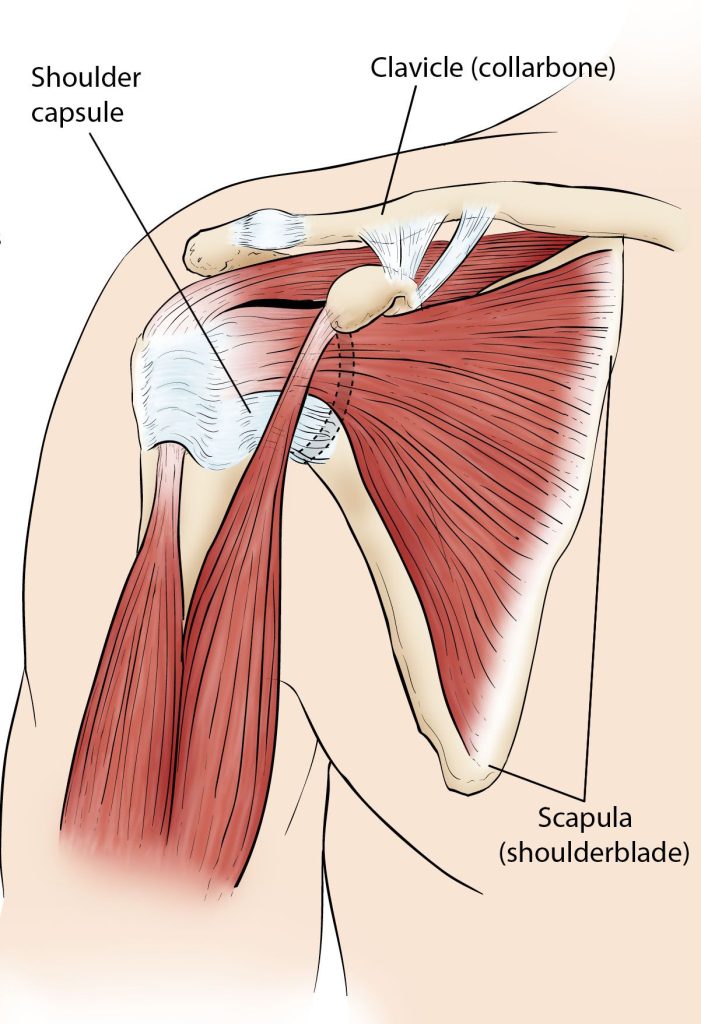
The brain and the tissues of the face are nourished by carotid arteries that are situated on either side of the neck.
A plaque that forms inside the inner carotid walls as a result of the accumulation of fat, cholesterol, and other particles can constrict the artery.
This narrowing, known as stenosis, is risky because it restricts blood flow and oxygen to the brain and may result in a stroke. Detecting it at an early stage of development might also be challenging.
In a healthy individual, the increased heart rate that comes with exercise stabilizes the drag force acting on the artery wall. This lowers the likelihood of stenosis.
The authors of the study noted that for those already dealing with stenosis, the outcome might be different.
Exercise truly increases the risk of stroke?
According to Dr. Adi Iyer, a neurosurgeon and interventional neuroradiologist at Providence Saint John’s Health Centre in California, medical professionals have long recognized that having a greater resting heart rate increases a person’s chance of having a stroke.
Iyer argued that the study’s suggested link between exercise-induced elevated heart rate and stroke in individuals with moderate or severe carotid stenosis is novel “and still remains unclear.”
This study used computer modeling, which is not a perfect representation of actual human physiology. For instance, the circle of Willis, a system of collateral circulation in the human brain, joins the arteries that run from the left to right and front to back of the brain.
The stroke risk for actual patients will eventually be determined by the patency of these collaterals and a host of other variables, according to neurosurgeon Dr. Adi Iyer.
Iyer stated that “temporary weakness or numbness on one side of the face or body, or even temporary vision loss from one eye. This can be the most common signs of a narrowed carotid artery.”
“Patients should seek physicians’ recommendations on lifestyle modifications, including exercise regimens when there is a moderate or severe blockage in the carotid artery,” Iyer advised.
Patients should seek surgical consultations because there are now several extremely effective. Minimally invasive procedures are available to them for unblocking their obstructed carotid arteries.
Exercise with clogged arteries should be avoided.
Exercise is frequently advised to avoid cardiovascular disease, according to study author Dr. Somnath Roy, PhD, associate professor in the Department of Mechanical Engineering at the Indian Institute of Technology Kharagpur in India.
According to existing research, exercise-induced faster pulse rate reduces pressure on the arterial wall and delays the development of stenotic occlusion. Through our numerical projections, “we have seen similar characteristics for healthy arteries.”
The oscillatory shear index (WSS) showed increased oscillation levels for artery models with advanced stenosis or constriction, according to Roy.
The likelihood of additional stenosis advancement and extremely high shear stress may increase with higher levels of these oscillations.
If levels are very high, stenotic plaque may begin to fracture and form blood clots or emboli (a foreign body blocking an artery). This may travel to the brain, obstruct weaker blood arteries, and trigger a stroke.
“By using computer simulations based on physiologically relevant data, the authors have described the impact of higher heart rates on hemodynamics in healthy and stenosed carotid arteries. According to Dr. Joseph C. Maroon, clinical professor, vice chairman, and Heindl scholar in neuroscience at the University of Pittsburgh’s Department of Neurosurgery, “It is not clinical research.
“I find the observations interesting. They are arguing that stenotic lesions that are 50% or more likely to be obstructive of blood flow may be more likely to cause a heart attack or stroke.
According to Roy, the research team intends to examine the consequences of high heart rates at additional arterial models. This includes coronary artery, aorta, and others, in subsequent studies.
How stenosis is impacted by exercise?
As seen in the study, patients with moderate or more severe stenosis may experience negative effects from vigorous activity.
“Although flow volume is not reduced until an artery has 90% or greater stenosis. The suggestion is that the shear and flow disturbances caused by a 50% narrowing of an artery can disrupt the lining of the artery (the intima). Also, precipitate clotting and obstruction despite a normal flow,” Maroon said.
This is a crucial finding that requires confirmation and more research. It’s crucial to take into account any potential variations between a computer model and a human heart rate while learning more about the connection between exercise and stenosis.
“Substantial variability in human heart rate (as compared to a computer model) can occur during different-impact workouts, sports, and isometric exercises,” said Dr. Sandra Narayanan, a board-certified vascular neurologist, and neuro-interventional surgeon at the Pacific Stroke & Neurovascular Centre at the Pacific Neuroscience Institute in Santa Monica, California.
The length of sustained heart rate elevation and its detrimental effects on cerebrovascular risk in individuals with moderate-to-severe carotid artery stenosis are related. Although further research is required to fully understand this relationship.
Additionally, Narayanan said it would be useful to determine whether a particular activity is more likely to increase lifestyle risk. Also, if the risk is more closely linked to tachycardia and is independent of cause.
Conclusion
In patients with severely clogged carotid arteries, an elevated heart rate can result in a stroke, claims a recent study.
However, carotid stenosis is not very common in the general populace. Exercise keeps the blood flowing normally in patients with no or little obstruction.
For the majority of people, regular exercise continues to provide some of the best protection against heart disease. The relationship between exercise-induced heart rate and stenosis has to be further studied.
For individuals with moderate or more severe stenosis levels, experts advise walking, yoga, and balance exercises.
REFERENCES:
- https://www.medicalnewstoday.com/articles/exercise-may-increase-stroke-risk-for-people-with-blocked-arteries
- https://www.healthline.com/health-news/intense-exercise-may-raise-stroke-risk-people-with-blocked-arteries
For Stroke medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_99