Top treatment options for Lower respiratory tract infection
Infections of the lower respiratory tract (LRTI), which include the trachea and alveolar sacs, damage the airways (below the level of the larynx).
There are numerous methods to describe LRTI. Acute bronchitis, bronchiolitis, and influenza are examples of acute infections that affect the airways, while pneumonia is an example of an acute infection that affects the alveolar sacs.
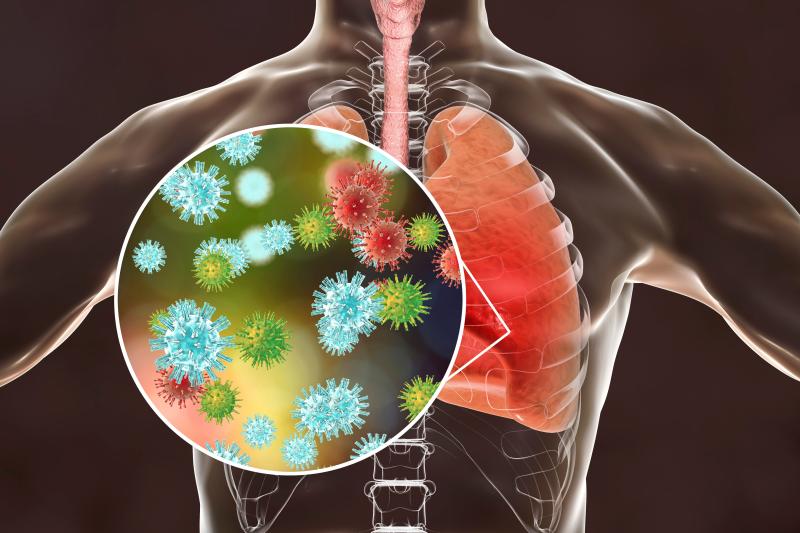
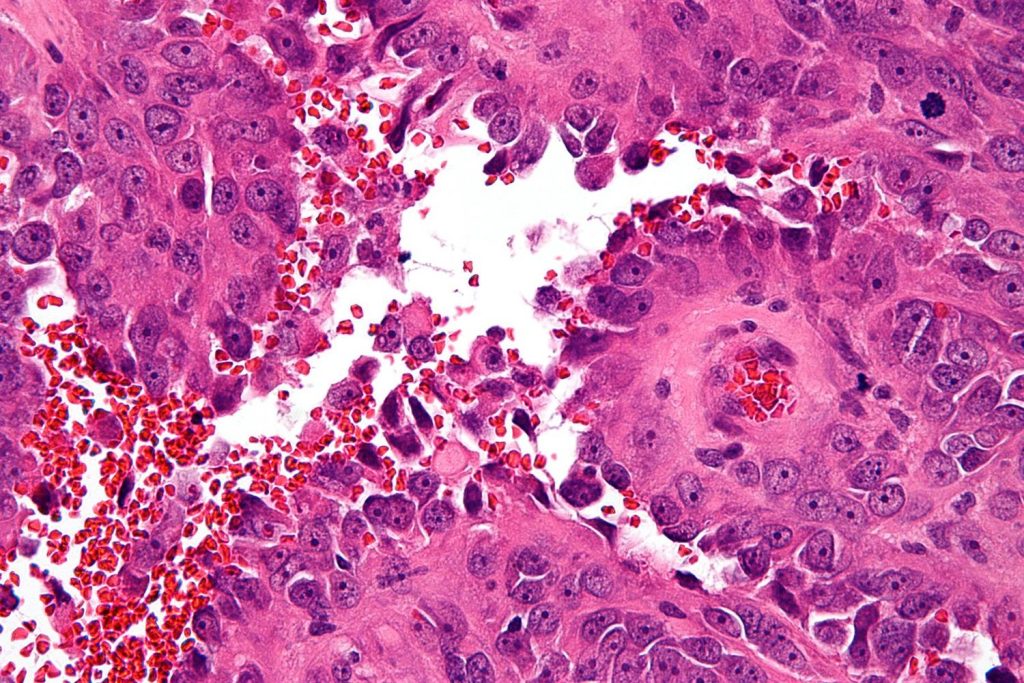
The most frequent causes of infections are the microscopic organisms known as bacteria or viruses. They are spread between people through coughing, sneezing, and occasionally by coming into indirect contact with surfaces in the form of microscopic droplets.
Antibodies are typically produced by infected individuals to combat the virus. If re-infected, the antibodies aid in fighting the same strain of illness. The body produces new antibodies in response to viruses’ ability to modify their appearance and manifest in many strains. These germs can occasionally progress to produce an LRTI.
Types of lower respiratory infections
The windpipe, big airways of the lungs, tiny airways of the lungs, and air sacs of the lungs make up the lower respiratory tract. The lower respiratory system plays a crucial role in the blood’s ability to receive oxygen. The lower respiratory tract may contract viruses and occasionally bacteria during the winter months. Several distinct lower respiratory illnesses are caused as a result of this.
A typical respiratory tract infection is bronchitis. It is described as an inflammation of the lung’s major airways. Although bronchitis can afflict people of any age, it often affects older children and adults. Bronchitis sufferers compare their condition to having a chest cold.
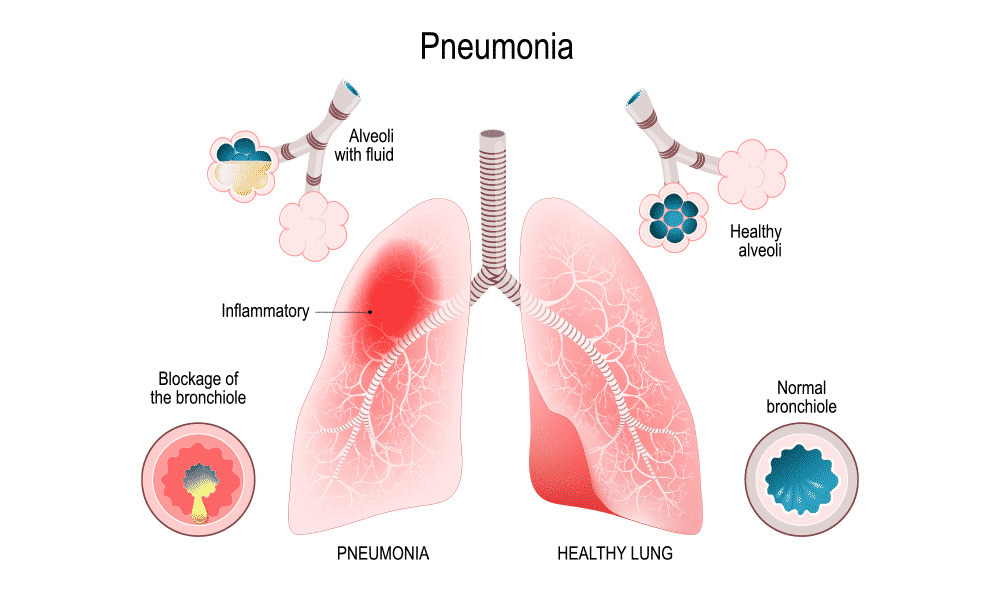
An infection of the lungs’ air sacs is known as pneumonia. Pneumonia can affect anyone at any age, but it can be particularly dangerous for infants, the elderly, and those with compromised immune systems. Pneumonia can have a variety of symptoms and a number of different causes.
Inflammation of the lungs’ tiny airways is known as bronchiolitis. Infants and toddlers under the age of two are more likely to contract this illness. During the fall and winter, bronchiolitis is one of the leading causes of hospitalisation in young children.
Causes of lower respiratory infections
Viruses that enter the respiratory tract are the main cause of lower respiratory tract infections. The next most prevalent cause is bacteria.
- The two viruses that cause bronchitis most frequently are influenza and the rhinovirus (which causes the common cold).
- Depending on the age group, a virus or bacteria may be the most frequent cause of pneumonia.
- The rhinovirus, respiratory syncytial virus (RSV), and human metapneumovirus are the most frequent causes of bronchiolitis.
In recent years, lower respiratory tract infections and occasionally pneumonia have been linked to SARS-CoV-2, the virus that causes COVID-19.
Symptoms of lower respiratory infections
Lower respiratory tract infection symptoms might vary depending on the infection’s severity. Common cold symptoms can also occur in less serious infections, such as:
- a congested or runny nose
- dried-up cough
- minimal fever
- minor throat discomfort
- chronic headache
Symptoms of more serious illnesses can include:
- a phlegmy cough that is extremely bad
- fever
- having trouble breathing
- skin with a blue tint
- quickly breathing
- a chest ache
- wheezing
Diagnosis
A lower respiratory infection is typically identified by a doctor during an examination after talking to the patient about their symptoms and how long they have been present.
Using a stethoscope, the doctor will monitor the patient’s respiration and chest during the examination. In order to diagnose the issue, the doctor could request tests like these:
- Using pulse oximetry, one may determine the blood’s oxygen content.
- X-rays of the chest to look for pneumonia
- blood tests to look for viruses and germs
- examining mucous samples for viruses and germs
Treatment
Some infections of the lower respiratory system resolve on their own. These less severe viral infections can be treated at home with:
- drugs available without a prescription for a cough or fever
- a plenty of sleep
- consuming a lot of liquids
A doctor might recommend extra treatment in other situations. This could involve breathing treatments like an inhaler or medicines for bacterial infections.
- A person could occasionally require a hospital visit to obtain IV fluids, antibiotics, or breathing assistance.
- Infants and very young children may require more care than older kids or healthy adults.
Infants with a higher risk of serious infections, such as premature infants or infants with congenital heart defects, are frequently monitored extra carefully by doctors. A doctor may be more likely to advise hospitalisation in these circumstances.
Patients 65 years of age and older, as well as those with compromised immune systems, may potentially benefit from the same kind of treatment, according to doctors.
Conclusion
Lower respiratory tract infections that are not difficult are completely curable in the majority of healthy people. Complications, however, could have long-term consequences.
People with other medical issues, seniors over 65, and young children under 5 are at the greatest risk for complications. These people can take precautions to avoid lower respiratory infections and seek medical attention if they experience any symptoms.
REFERENCES:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5846264/
- https://www.medicalnewstoday.com/articles/324413
- https://www.rileychildrens.org/health-info/lower-respiratory-tract-infection
- https://www.templehealth.org/services/conditions/lower-respiratory-tract-infections
- https://www.goodrx.com/conditions/lower-respiratory-infection/what-is-a-lower-respiratory-infection
For more details, kindly visit below.