What are the causes and symptoms of Corona Virus?
A lot of medical professionals think that pangolins or bats are where the new coronavirus strain most likely got its start. The initial human transmission occurred in Wuhan, China. Since then, person-to-person contact has been the primary method of viral transmission.
A class of viruses known as coronaviruses can infect both humans and animals with sickness. One example of a coronavirus is the SARS-CoV virus strain, which causes the severe acute respiratory syndrome (SARS). In 2002–2003, SARS spread quickly.
The severe acute respiratory syndrome coronavirus 2 is the name of the new coronavirus strain (SARS-CoV-2). Coronavirus illness is brought on by the virus (COVID-19).
Approximately 80% of COVID-19 patients recover without specialised care. These individuals could have minor flu-like symptoms. However, 1 in 6 individuals may develop serious symptoms, such as breathing difficulties.
What is a Corona Virus?
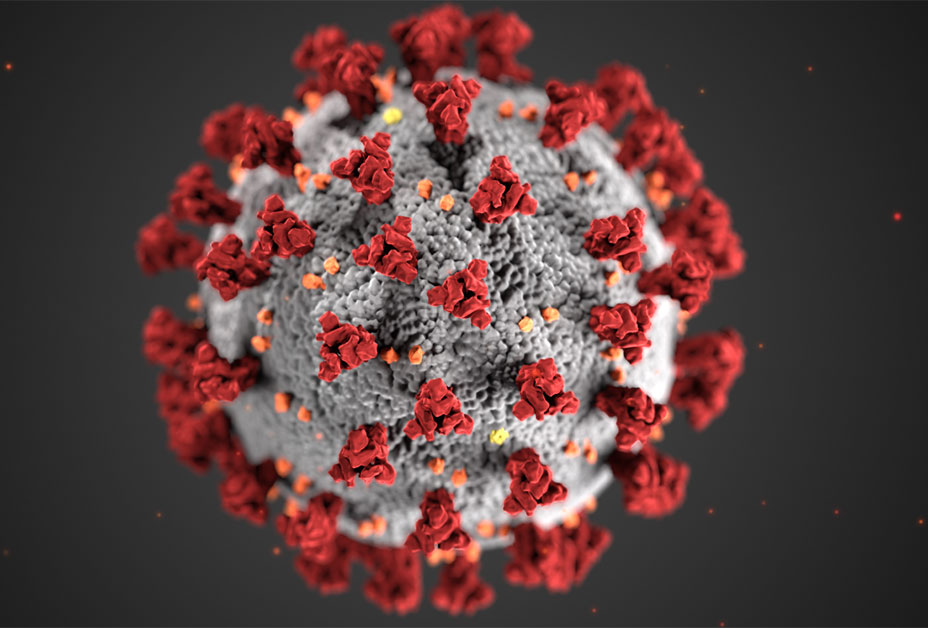
A group of viruses known as coroviruses can make people sick with respiratory conditions. Because the virus’s surface is covered in spikes that resemble crowns, they are known as “corona.” Examples of coronaviruses that affect people include the severe acute respiratory syndrome (SARS), Middle East respiratory disease (MERS), and the common cold.
What caused coronavirus?
Wuhan, a city in China’s Hubei region, was the site of the most recent outbreak. In December 2019, the first COVID-19 cases were reported.
Certain animal species, including cattle and camels, frequently contract coronaviruses. Despite the rarity, coronaviruses can occasionally be transmitted from animals to people. According to a reliable source, this new strain most likely originated from bats, while one study raises the possibility that pangolins were the original host.
It is still unknown how the virus originally infected humans, though. According to some reports, the first cases originated at a seafood and livestock market in Wuhan. SARS-CoV-2 may have begun to spread to humans from this location.
How it spreads?
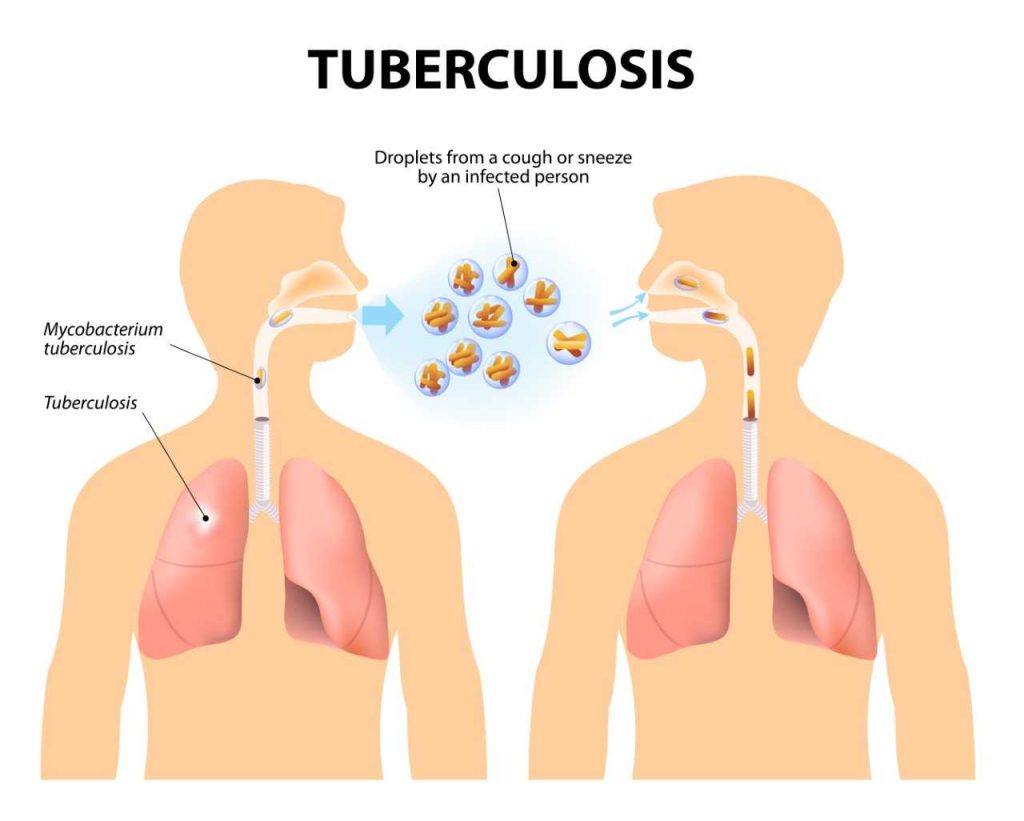
Through small communities, SARS-CoV-2 transmits from one person to another. People who have COVID-19 cough or exhale little droplets containing the virus. These droplets can cause an infection if they go into someone’s mouth or nose who doesn’t have the virus.
Close contact with an infected person is the most typical way that this disease spreads. Close proximity is approximately 6 feet. When a person’s symptoms are the worst, the disease is most contagious. But even someone who is symptom-free can transfer the infection. According to a recent study, 10% of infections come from persons who don’t have any symptoms.
The virus may also droplets that land on neighbouring surfaces or objects. By touching these surfaces or objects, other people could contract the infection. If the person then touches their mouth, nose, or eyes, infection is probably going to occur.
It is significant to note that research on COVID-19 is still in its early stages. The new coronavirus may be spread through additional channels as well.
Symptoms and Complications
The symptoms of COVID-19 infection might range from little to no symptoms to serious sickness and death. Most illnesses start up to 14 days following exposure and are typically mild.
The most typical signs are:
- a new or worsening cough
- Fever
- Tiredness
- Chills
- muscle pain
- Headache
- diarrhoea, vomiting, or nauseous
Additional signs include:
- respiratory issues or shortness of breath
- unwell throat
- swallowing that hurts or is challenging
- eye colour (conjunctivitis)
- a diminished appetite
- loss of flavour or scent
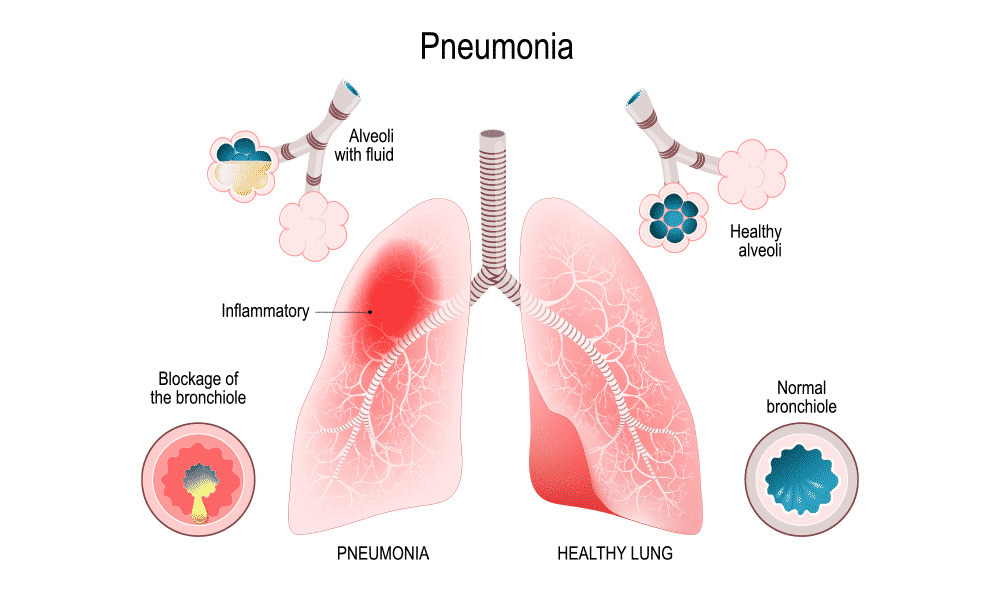
Some individuals, nevertheless, could experience other, more serious consequences like pneumonia or respiratory failure. People who are not fully immunised, pregnant women, adults 60 and older (risk rises with age), people with underlying chronic medical conditions (such as heart disease, diabetes, lung disease), people who are obese with a BMI of 40 or higher, and people with weakened immune systems are at higher risk of developing a severe illness from COVID-19.
In certain instances, COVID-19 infection might result in chronic symptoms that persist for several weeks or months after the patient has recovered. This is referred to as a lengthy COVID or a post COVID-19 condition. Regardless of the severity of your infection or whether you have symptoms, you could develop post-COVID-19 illness.
Symptoms that commonly affect adults include:
- Tiredness
- memory issues
- trouble sleeping
- breathing difficulty
- Concern and sadness
- general discomfort and suffering
- having trouble focusing or thinking
- Posttraumatic stress disorder (PTSD)
Typical signs that children experience include:
- Tiredness
- Headaches
- Loss of weight
- muscle ache
- trouble sleeping
- runny or stuffed nose
- having trouble focusing or thinking
REFERENCES:
- https://www.mayoclinic.org/diseases-conditions/coronavirus/symptoms-causes/syc-20479963
- https://my.clevelandclinic.org/health/diseases/21214-coronavirus-covid-19
- https://www.who.int/health-topics/coronavirus
- https://medbroadcast.com/condition/getcondition/covid-19
- https://www.medicalnewstoday.com/articles/coronavirus-causes
For more details, kindly visit below.